
Superior Index Go to the next: Chapter 11
Print Files: A4 Size.
Fibrinogen is a large sticky protein molecule that's intimately involved in blood clotting and inflammation management. It's manufactured by your liver.
Fibrinogen, a soluble protein, floats in the bloodstream. If bleeding occurs, it is transformed into a solid fibrous protein that becomes the scaffolding upon which a blood clot is formed. As a completely separate function, fibrinogen also functions as a messenger molecule that coordinates and regulates our bodies' response to inflammation.
We need fibrinogen. Like homocysteine, C-reactive protein, and cholesterol, this molecule - at normal levels - performs necessary and important functions in the human body. When we make too much of it, problems appear and these problems - as we shall see - have to do with clotting and inflammation.
Many studies have shown that elevated fibrinogen is a major risk factor for atherosclerosis; cardiovascular disease specialists no longer question its importance. Several decades of research have confirmed that persistently elevated fibrinogen levels predict heart attacks and strokes with exceptional accuracy. It is easy to see why this would be true: fibrinogen participates in just about every step along the way to developing an atherosclerotic blockage in the vascular system.
Many experts feel that fibrinogen may be the overall single best risk factor for predicting heart attacks and strokes. One prominent researcher has stated that an elevated fibrinogen raises heart disease risk by 600 to 900 percent. Elevated fibrinogen levels have also been linked to increased risk of diabetes, hypertension, and even cancer. Several researchers have shown that a high fibrinogen is associated with a sevenfold increase in deaths from all causes. Maintaining a normal fibrinogen level thus translates into huge health dividends.
Fibrinogen is no innocent bystander that just happens to be hanging around when other factors cause vascular disasters. Fibrinogen, at normal (or "physiologic") levels, behaves itself. Too much fibrinogen, however, and it morphs into a monster that actively participates in the cellular destruction that leads to cardiovascular disease. At levels exceeding 250 mg/dL, fibrinogen launches attacks on the vascular endothelial lining and on the clotting system.
By causing exaggerated inflammation fibrinogen destroys the endothelium. This promotes atherosclerosis.
By promoting clot formation, excess fibrinogen obstructs major vessels These local clots can become deadly blood vessel-blocking thrombi.
Fibrinogen's one-two combination punch of inflammation and clot promotion causes strokes and heart attacks. Yet, ironically, very few doctors order this test and even fewer know how to coax an elevated fibrinogen down into the normal range.

Here with me now in my consultation room is long time friend and patient Brent Chadwick, a 48-year-old San Francisco assistant district attorney. Vibrant, outgoing, and not without a sense of humor, Brent's a crusty barrister who's accustomed to adversarial courtroom dramatics, so instead of asking questions like a normal patient, he grills me as if I were a defendant. All he really wants is the truth.
I tested Brent's heart markers a few weeks earlier, and he's here to discuss the results. The only abnormal result on his Cardiovascular Risk Profile is an elevated fibrinogen.
"Doc, I Googled fibrinogen, and now I know that it's a clotting protein and an `acute phase reactant.' Whatever that is. What does any of that have to do with my heart?"
"Well, Brent, fibrinogen is an important independent causative marker for atherosclerosis and coronary heart disease. In other words, high levels of fibrinogen predispose a person to heart attacks and strokes, even though - as is true for you - cholesterol and all the other risk factors are normal."
"Since everything else was normal on your battery of tests, how bad could it be? Couldn't we just give me a pass on this one?"
"Sorry, Brent, but there is a reason we call these `independent markers.' It's because they act independently of one another. In other words an isolated fibrinogen elevation (or CRP or glucose or homocysteine or LDL) can and will cause atherosclerotic heart and cardiovascular disease all by itself.
"And just how good a marker is it?" he asks, in low, even, lawyerly tones.
"A very good one. High fibrinogen levels have at least as great a predictive value as any other marker. In fact elevated fibrinogen accounts for many of the heart attacks that happen to the 50% of heart attack victims who have healthy cholesterol levels. One major study involving over 2000 men showed that those with a low LDL cholesterol but high fibrinogen levels had six times the risk of a myocardial infarction than those with a low fibrinogen and elevated cholesterol."
"Yes, it is. Of course if both cholesterol (or any other marker) and fibrinogen are elevated, one's risk is very much higher than if it's just one or the other."
"What's my fibrinogen level doc?"
"At 341, it's well above the upper limit of the ideal range (150-250 mg/dL), and this tells me that you are at risk."
"It is a very large protein molecule that commands a lot of respect."
"Respect? Do proteins get respect?"
"This one sure does. It can both save your life and it can kill you."
"Normal levels of fibrinogen are important for blood clotting and managing inflammatory challenges to your body such as infections, allergies, and stress. But at high levels, fibrinogen morphs into a vandal. It damages arteries, accelerates atherosclerosis, encourages the formation of blood clots ... "
"You mean the kind of clots that cause heart attacks?"
"Yes, but not just those, all kinds. Fibrinogen doesn't know the difference between a heart attack and a cut finger ... "
"I sure would if I were the one having a heart attack!"
"Well, Brent, I guess that proves you're smarter than fibrinogen."
"I just kept going: `Fibrinogen, you see, regardless of its IQ, floats along in the bloodstream as a soluble protein. When bleeding occurs, fibrinogen's job is to plug the leak, and to accomplish this it possesses the unique capacity to change from its usual soluble form into an insoluble form called fibrin. Fibrin is sticky, so it adheres to the inside endothelial surface of the blood vessel forming the mesh-like matrix or scaffold upon which a blood clot can be built. It then snares passing red blood cells and platelets, forming a clot. Now if you have cut your finger, it is important that the coagulation process I just described occurs rapidly so you don't lose much blood. If you are hemorrhaging, fibrinogen can save your life. Too much fibrinogen can cause a disaster, though, by enhancing the probability of an unwanted clot that blocks blood flow to your heart or brain. That's why too much fibrinogen dramatically increases your risk of a heart attack or stroke. We want to avoid this at all costs.' "
"We sure do! So, does it really cause heart attacks, or is it just hanging around when they happen?"
"Brent apparently now needs to determine whether fibrinogen is an innocent bystander or the actual killer. This is an excellent question."
"Fibrinogen participates in the process. It has been clearly recognized to be a killer. Let me put it this way, Brent: at the right level in your system, fibrinogen is a hero committed to protecting your life. Too much, however, and our savior mutates into a homicidal maniac."
"An `aha' smile creeps onto Brent's face, and I can tell that this is a way of putting it that he can wrap his legal mind around. Now he is going to start looking for the smoking gun."
"But you haven't told me exactly how it causes heart attacks and strokes. Since my level is elevated, I have a vested interest in your answer."
"Fibrinogen is involved at several different points. It causes endothelial irritation and inflammation. (See Chapter 5, Atherogenesis: How Arteries Fail.) It then continues to participate by incorporating itself into arterial plaque as it forms. Inside the wall of the artery, fibrinogen converts to its insoluble form, fibrin, which then serves as the scaffold that holds cholesterol in plaque. Fibrinogen is also incorporated into the foam cells that contribute to plaque.
"Outside the plaque, in the bloodstream, excess fibrinogen will increase the viscosity of blood, causing it to slow down - and when blood stagnates it is then more likely to clot."
"Kind of like when there's congestion on the freeway?"
"Why, yes, but then fibrinogen raises the ante by encouraging platelets to stick together (this is called platelet aggregation) where and when the traffic slows down. When platelets clump, you have a clot. This impairs local circulation and shuts off the local supply of oxygen and food to cells in the heart or brain. At its worst it can cause an abrupt total blockage of blood flow in that artery. That can spell sudden death."
"Brent, these kinds of arterial blood clots are the leading cause of death in the Western world. Every year in the U.S. alone, about 1,000,000 heart attack and stroke deaths occur as a result of blood clots obstructing the delivery of blood to the heart or brain."
"So I guess taking steps to reduce elevated levels of fibrinogen makes a lot of sense - perhaps could save one's life? Perhaps my life! Perhaps the lives of many many others."
"Millions of lives would be saved if doctors routinely tested and treated it!"
"Why not? That'd be malpractice, wouldn't it?"
"One would think so, Brent, since we are talking about a marker far superior to the cholesterol we doctors routinely - almost religiously - check."
"Doctors are unlikely to order a fibrinogen level because if it came back high, they wouldn't know what to do. When they spot a high cholesterol, they can write an Rx for statin drugs. But there is no `statin' for fibrinogen." If a fibrinogen-lowering drug existed, you'd see medical journal ads, continuing education programs, research money for population studies, free samples, TV commercials - the whole enchilada. Unfortunately, however, the only medications that lower fibrinogen are plant-derived, food-based medicines. Big Pharma can't patent these `nutraceuticals.' With no prospect for profits, there's no incentive to market natural products like nattokinase (a soybean derivative), curcumin, serrapeptase, bromelain, green tea, or garlic."
"I see. So the docs just refuse to order the test?"
"Yes. When asked to order a fibrinogen level, Brent, most doctors will tell you it's is a "newly identified" risk factor, so they need "more proof" before they'll order it. Fact is, hundreds of studies over the past thirty years have documented fibrinogen's status as a major risk factor. No cardiovascular expert now questions fibrinogen's atherogenic potential or its predictive power for heart attacks and strokes. It's an honest-to-goodness smoking gun for strokes and myocardial infarctions."
"And natural medicines do work to lower fibrinogen?"
"Yes, Brent. The ones I just mentioned are proven nutritional medicines that either lower fibrinogen or protect from its adverse effects, or both. Before we get you started on a program, however, let me explain a little more about what fibrinogen is and why it is important ... "
If one were to step back and scan the entire molecular biological landscape in search of the hottest smoking gun - the factor most intimately associated with heart attacks and strokes - one biochemical would stand out above a crowded field: fibrinogen. Why? Because fibrinogen is intimately associated with - and the driving force behind - inflammation and blood clot formation, the two processes that cause strokes and heart attacks. Fibrinogen directly causes inflammatory damage to the wall of the artery, setting the stage for atherosclerotic plaque and thrombus formation. And, in heart attacks and strokes, fibrinogen (a liquid) solidifies to form fibrin, resulting in an artery-blocking clot. The connection doesn't get any more intimate than that.
Fibrinogen has two main jobs in the human body. The first is as an inflammatory protein, an "acute phase reactant". Inflammation anywhere in the body triggers hepatic fibrinogen production. This protein is released and travels far and wide notifying various body systems that inflammation is afoot and providing explicit instructions about how to deal with it. Problem is, fibrinogen doesn't just manage inflammation; at elevated levels, it also causes inflammation. Elevated fibrinogen levels damage blood vessels, setting the stage for heart attack and stoke.
Fibrinogen's other job is to serve as the soluble precursor of fibrin, the solid protein that forms the scaffolding upon which a blood clot is built. Damage to an artery triggers the conversion of fibrinogen to fibrin, thus initiating a blood clot. This clot is usually necessary; our blood vessels are continuously sustaining damage from trauma (e.g. your daily workout) plus normal wear and tear. Local clotting is the first step in the healing process. These "healing clots" are short-lived, remain small, and serve to quickly restore the healthy artery wall. However, when arterial damage is sustained, regardless of cause, the clot may increase in size and become a thrombus - a larger, growing clot that can block a blood vessel. Excess fibrinogen increases the propensity to make clots. Not a good thing. Lower fibrinogen levels are associated with protection from unwanted clots.
Coagulation - the clotting of blood - is a complex sequence of biochemical transformations initiated by tissue damage and terminating with the formation of a blood clot. That clot's purpose is to plug the hole and stop the bleeding. Coagulation is a tightly controlled process that protects us from excessive bleeding. In the final step of the cascade, fibrinogen (a soluble protein) is converted into insoluble fibrin, the long thin fibers that intertwine, forming a mesh that traps platelets and red blood cells to form a clot.
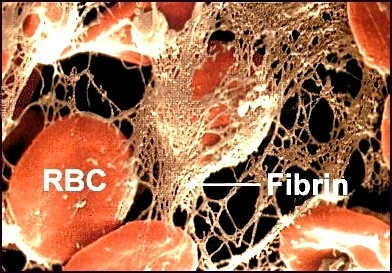
It is crucial that our bodies maintain a dynamic homeostatic balance between fibrinogen and fibrin within the clotting system. Fibrinogen is always changing into fibrin, but the fibrin formed is continuously dissolving and being recycled back into fibrinogen, so no clots form. As long as fibrinogen levels don't get too high, this system works great. When this recycling process breaks down, however, fibrinogen levels go up. The excess fibrinogen irritates the arterial endothelial lining and damages it, causing local inflammation. Fibrinogen converts to fibrin and sticky fibrin fibers accumulate, providing a scaffold on the inside lining of the arterial wall that traps platelets and red blood cells to form a clot. This local injury and clot attract oxidized LDL- cholesterol, monocytes, cellular waste products, and an array of inflammatory molecules that coalesce into atherosclerotic plaque.
If the surface of a developing plaque continues to be irritated, the plaque grows in size and may rupture, causing more fibrinogen, platelets, RBCs, and other inflammatory chemicals to accumulate at the site in an attempt to repair the injury. Under these conditions, the local clot grows larger and becomes a thrombus which gradually narrows and chokes off flow in the artery.
A thrombus might not initially block blood flow, but if a piece breaks off and travels downstream (now we call it a thromboembolism), it will come to rest in a narrower part of the vessel, where it completely chokes off the flow of blood, causing rapid tissue death and sudden, severe symptoms of a myocardial infarction or stroke. At this point, more often than not, someone dials 911.
Besides clotting, fibrinogen has another main job, that of initiating, monitoring, and managing the inflammatory process.
You may have already noticed that life in a human body entails a more or less continuous onslaught of assaults coming from many directions. Just using our bodies to move around creates wear and tear on the joints, ligaments, tendons, and muscles. Add to that physical injury (trauma), microbial attack (we are continuously fighting off pathogens), allergens (most of us have food or inhalant allergies), and toxins (we do survive in a toxic environment).
Without a way to respond to all this damage we'd be in big trouble. Fortunately we (or, more specifically, our bodies) do have a "plan". Our response to all the different kinds of assault - trauma, infection, allergy, and toxins - is inflammation. Inflammation, in turn, triggers what pathophysiologists call the "acute phase response" or "APR". The purpose of the APR is to manage the inflammatory reactions, to respond to the damage, and to manage the healing process. The APR consists of an outpouring from the liver of a barrage of inflammation-managing "acute phase" proteins. The list of known APR proteins is very long and you have probably not heard of most of them: ceruloplasmin, serum amyloid A, alpha-1 antitrypsin, haptoglobin, interleukin (IL)-1 receptor antagonist, components of the complement cascade, hepcidin, ferritin, C-reactive protein ... and our friend fibrinogen. Collectively these APR proteins provide enhanced protection against invading micro-organisms, limit tissue damage, enhance healing, and promote a rapid return to homeostasis.
We need the APR to handle difficult situations; it temporarily improves our adaptive and defensive capabilities. Next time you catch a cold, cut or bonk a finger, or develop a splitting headache, you can impress all your friends by telling them you have decided to have an APR. Not that there's actually a choice here. Literally anything that causes inflammation (including trauma, infection, toxins, allergens, arthritis, myocardial infarction, stroke, and various cancers) will cause a shift to the APR and heightened fibrinogen production.
Think of fibrinogen as like a herd of tiny horses, each one ridden by a little Paul Revere. When there's inflammation anywhere in your body, hepatic fibrinogen production increases, and gobs of it are released into the bloodstream. They float to the far-flung regions of your body shouting "Inflammation is coming! Inflammation is coming!"
The walls of blood vessels in the heart are especially sensitive to these fibrinogen messages. Prolonged levels exceeding 250 mg/dL cause the endothelial damage that initiates formation of both atherosclerotic plaque and thrombi.
Two chapters in this book are devoted to acute phase reactants: C-reactive protein, and fibrinogen - the two that also happen to be heart markers. This is not a coincidence.
Sooner or later all of us will experience an elevated fibrinogen because we all get transient inflammation. We stub our toe, twist an ankle, shovel too much snow, play that extra set of tennis, have surgery, get a toothache, sinus infection, cold, or flu (infection). When we heal, the inflammation subsides, and the fibrinogen level comes down. The very presence of an elevated fibrinogen is synonymous with danger and damage. When considering cardiovascular risk, however, we are not interested in transient elevations. It's only a prolonged high fibrinogen level that causes atherosclerosis.
The only way to know if a fibrinogen elevation is acute or chronic is to test again (usually in 1-3 months). If fibrinogen is normal on repeat testing, we know it was a transient elevation and there is no need for concern. If it remains elevated, regardless of the cause for the elevation, treatment is necessary because persistent elevation causes arterial damage. Optimally, one would identify and treat the cause, but if that is not possible, it is still necessary to address the elevated fibrinogen and lower it with nattokinase, curcmuin, and/or serrapeptase.
Researchers have discovered a biologically sadistic turn of events - if fibrinogen is elevated along with any other heart marker, atherosclerosis and heart attack risk skyrockets. Here's how fibrinogen works in cahoots with the other heart markers:
Reduce fibrinogen level to 250 mg/dL or less.
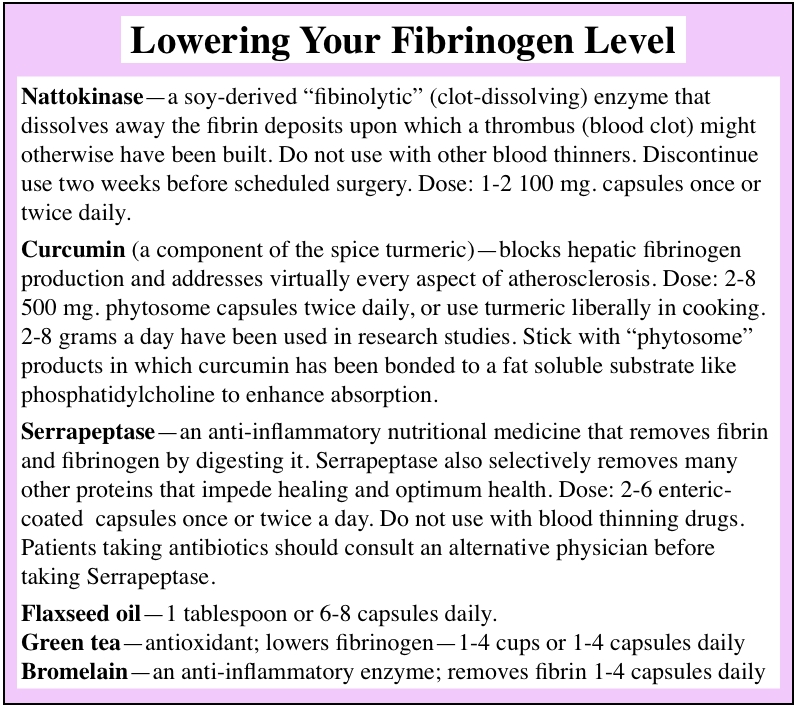
Nattokinase - a soy-derived "fibinolytic" (clot-dissolving) enzyme that dissolves away the fibrin deposits upon which a thrombus (blood clot) might otherwise have been built. Do not use with other blood thinners. Discontinue use two weeks before scheduled surgery. Dose: 1-2 100 mg. capsules once or twice daily.
Curcumin (a component of the spice turmeric) - blocks hepatic fibrinogen production and addresses virtually every aspect of atherosclerosis. Dose: 2-8 500 mg. phytosome capsules twice daily, or use turmeric liberally in cooking. 2-8 grams a day have been used in research studies. Stick with "phytosome" products in which curcumin has been bonded to a fat soluble substrate like phosphatidylcholine to enhance absorption.
Serrapeptase - an anti-inflammatory nutritional medicine that removes fibrin and fibrinogen by digesting it. Serrapeptase also selectively removes many other proteins that impede healing and optimum health. Dose: 2-6 enteric-coated capsules once or twice a day. Do not use with blood thinning drugs. Patients taking antibiotics should consult an alternative physician before taking Serrapeptase.
Flaxseed oil - 1 tablespoon or 6-8 capsules daily.
Green tea - antioxidant; lowers fibrinogen - 1-4 cups or 1-4 capsules daily
Bromelain - an anti-inflammatory enzyme; removes fibrin 1-4 capsules daily

Fibrinogen floats harmlessly in the bloodstream as a soluble protein, until it encounters chemicals that signal the need for a clot (such as those it would encounter in an inflamed endothelium). These transform it into its insoluble form: fibrin. Thick bands of fibrin stick to the endothelial wall forming a meshwork that snags passing red blood cells and platelets, becoming a blood clot. This clot is positioned exactly where we don't want one: inside a blood vessel.
Nattokinase to the rescue! Nattokinase, a soy-derived dietary supplement and "fibinolytic" (clot-dissolving) enzyme, dissolves away excess fibrin deposits. This removes the fibrin scaffold upon which a thrombus could have been built. In the presence of nattokinase, thrombi (built on a fibrin scaffold), gradually shrink and disappear. Scientists call this "thrombolysis" - literally the "lysing" (or dissolving) of a thrombus. No prescription drug medication - not even Coumadin - is capable of thrombolysis.
Used safely in Japan for over 1000 years, nattokinase thins blood and outperforms pharmaceutical agents such as warfarin (Coumadin), Plavix, and heparin which merely thin the blood but are not capable of dissolving preexisting thrombi.
Taking nattokinase on a daily basis keeps fibrin under control and dissolves developing thrombi, thus preventing and reversing atherosclerosis. The risk of heart attack or stroke is dramatically reduced.
Research studies have shown that nattokinase is effective for a broad range of disorders including hypertension, peripheral vascular disease, intermittent claudication, hemorrhoids, varicose veins, chronic inflammation, pain, fibromyalgia, chronic fatigue syndrome, poor healing, retinal pathology, infertility, uterine fibroids, and endometriosis.
The beauty of nattokinase is that it delivers the clot-busting benefits of powerful drug medicines like heparin, tPA (tissue plasminogen activator), urokinase, Plavix, and warfarin (Coumadin) without any side effects or adverse reactions. Anti-clotting drugs interfere with normal function, whereas nattokinase supports and improves the overall health and functionality of the clotting system. This food-based medicine - free of side effects and toxicity - supports Mother Nature rather than working against her.
There have been no published reports of toxicity associated with nattokinase. A natural component of the soy food natto, nattokinase has been part of the Japanese diet for hundreds of years. For 30 years nattokinase has been used as a natural medicine in concentrations (i.e., doses) similar to those consumed in food with no side effects or adverse reactions. Do not combine nattokinase with drug blood thinners - e.g., aspirin, Coumadin (warfarin), or heparin. Patients taking blood thinners should consult their alternative health care practitioner before taking nattokinase. Pregnant women, breast-feeding mothers, and people with bleeding disorders should not take nattokinase. As with other anticoagulants, discontinue two weeks before scheduled surgery.
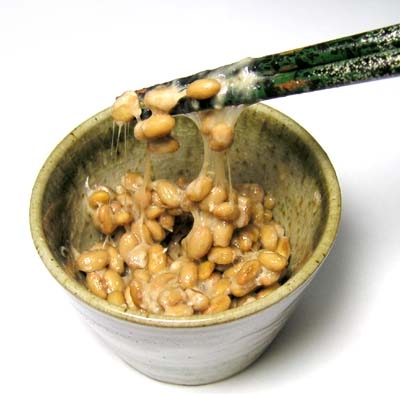
If you choose just one nutritional medicine to lower your fibrinogen, make it nattokinase.
Don't worry if your nattokinase doesn't cause your fibrinogen level to go down. Nattokinase does not block fibrinogen production; instead, it dissolves the solid fibrin strands formed from soluble fibrinogen, so it won't always lower fibrinogen levels, but it will still be protecting you from excess fibrinogen.
Take 1-2 100 mg capsules twice daily.

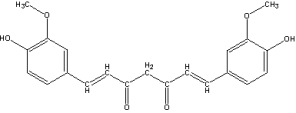
Curcumin (curcumin longa) is the bright orange-colored active ingredient in the popular native Indonesian and South Indian spice, turmeric. Think curry here. Curcumin contains potent antioxidant and anti-inflammatory compounds that block hepatic fibrinogen production.
Curcumin also addresses and reverses several other molecular biological changes that set the stage for stroke, heart attack, and hypertension.
Curcumin also protects against the adverse effects of too much fibrinogen by blocking "platelet aggregation". (Platelets, the blood clotting cells, normally float freely in the bloodstream, but right before a clot forms, they start hanging out in clumps - or aggregates.)
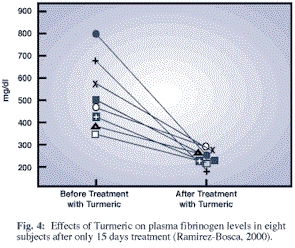
Curcumin addresses virtually every aspect of atherosclerosis
An elevated fibrinogen level (over 250 mg/dL) represents the tip of a large and complex iceberg of molecular responses and interconnected vascular changes, most of which, amazingly, are addressed by curcumin. Allow me to try to describe the complex set of events addressed by curcumin. By the time fibrinogen has become elevated, the inflammatory response is in full swing, and the stage is set for a stroke or a heart attack. Pro-inflammatory biochemicals like fibrinogen are being manufactured and released by the liver and endothelium and have flooded the system. The blood is thicker and more likely to clot. Platelets (our blood clotting cells) have been "activated" - that is, they are more likely to participate in the formation of a clot. Fibrinogen is ready to morph into fibrin and fibrin digesting enzymes have been deactivated so that fibrin is more likely to form. Vascular smooth muscle has now begun to proliferate and the arterial wall is thickening. LDL particles are being oxidized by the excess of free radicals generated by the inflammatory response. Oxidized LDL particles have launched a vicious and prolonged attack on the vascular endothelium and the media beneath it. While this attack is being waged, thrombi are very likely to form inside the vessel.
Mother Nature has conjured up a "dream herb" for reversing atherosclerosis and preventing heart attacks and strokes. Curcumin addresses every single one of the steps enumerated above. It reverses the inflammation, heals the damaged endothelium, thins the blood, reverses platelet activation, prevents oxidation of LDL, and blocks thrombus formation.
Broad spectrum cardiovascular effects
Researchers have shown that curcumin exerts the following vascular effects:

An anti-aging, optimum health bonanza
Beyond its vascular effects, curcumin displays a remarkable array of healthful, curative, even life-extending properties. Hundreds of research studies have documented the following medicinal and anti-aging effects:
Osteoarthritis (and other inflammatory) pain relief
In a study of 107 patients suffering from osteoarthritis of the knee, two grams of curcumin extract daily for six weeks achieved slightly better pain reduction scores than subjects given 800 mg of ibuprofen. Over 90% of the curcumin patients reported satisfaction, as compared to 80% for the ibuprofen users.
Several recent studies examining brain neurochemistry and cognitive functioning showed that curcumin increased levels of the mood-related neurotransmitters serotonin and dopamine. The herb also was found to enhance the effectiveness of antidepressant drugs by inhibiting levels of the enzyme monoamine oxidase. Animal studies have shown that curcumin reduces levels of the stress hormone corticosterone, reverses chronic stress-induced cognitive dysfunction, and improves memory.
2-8 500 mg capsules twice daily, or use turmeric liberally in cooking. 2-8 grams a day have been used in research studies. Curcumin is not well-absorbed. Purchase only "phytosome" products in which curcumin has been bonded to a fat soluble substrate like phosphatidylcholine to enhance absorption.
Serrapeptase (serrapeptidase, Serratia peptidase), a proteolytic (protein-digesting) enzyme, is an anti-inflammatory nutritional medicine that dissolves plaque, and removes both fibrin and fibrinogen by digesting them. Serrapeptase also selectively removes many other proteins that impede healing and optimum health.
With a long history of safe and effective use in Asia and Europe, serrapeptase has established itself as a reliable treatment for virtually all disorders in which pain, infection, and/or inflammation are prominent features. It is free of side effects or adverse reactions.
Serrapeptase seems almost too good to be true. How can one natural medicine dissolve arterial plaque, digest away blood clots (including thrombi), prevent atherosclerosis, alleviate arthritic and neuropathic pain, reverse inflammation, reduce edema (swelling and fluid retention), speed up healing and tissue repair, and remove scar tissue? The key to understanding how Serrapeptase could have such a broad spectrum of activity is that, as a proteolytic enzyme, it digests away unwanted proteins; it selectively digests away non-living tissue without harming living tissue. These properties address the essence of healing and regeneration of damaged tissue. Serrapeptase somehow "knows" the difference between necessary proteins (which comprise many of the most important structures in our bodies) and proteins that are unnecessary and unwanted (such as fibrinogen, fibrin, blood clots, atherosclerotic plaque, unwanted mucus, proteins that cause arthritic swelling and pain, other inflammatory proteins, and even scar tissue). Serrapeptase selectively removes the unwanted proteins, leaving all essential structures intact.
Serrapeptase was originally discovered centuries ago by Chinese Traditional Medicine herbalists. Technically known as Serratia peptidase, serrapeptase is produced by Serratia mercesans, a bacterium that populates the silkworm's digestive system. The enzyme is regurgitated by the moth when, after metamorphosis, it is ready to digest its way out of its cocoon - which happens to be made of an "unwanted" protein: silk!
At its core, atherosclerosis is an inflammatory condition in which endothelial irritants (see list in Chapter 5) trigger an inflammatory response in the arterial wall. Serrapeptase digests away the irritating proteins, thus reducing local inflammation. Serrapeptase outshines anticoagulant and anti-inflammatory drugs in that it dissolves the fibrin deposits and related inflammatory proteins that would otherwise become vessel-blocking plaque and thrombi. No drug can do that.
Anti-inflammatory, blocks pain, non-toxic alternative to pain-relievers
Because it can prevent the release of pain-inducing amines (such as bradykinin) from inflamed tissues, Serrapeptase relieves pain in a wide assortment of conditions, including osteoarthritis, rheumatoid arthritis, trauma, back pain, cervical pain, bursitis, muscle spasm, bone spurs, headaches, neuropathy, post-surgical pain, and just about any other disorder that involves inflamed and painful muscles, nerves, ligaments, and tendons. Physicians throughout Europe and Asia use serrapeptase as a harmless, side effect-free alternative to toxic drugs such as ibuprofen, salicylates, and other NSAIDs.
Promotes respiratory and sinus health
By digesting away the excess mucus secretions and scar tissue that block airways and lead to infection, serrapeptase has been successfully applied in a variety of respiratory conditions including asthma, rhinitis, sinusitis, otitis, chronic bronchitis, bronchiectasis, emphysema, chronic obstructive pulmonary disease (COPD), and cystic fibrosis.
Healing from injuries, infections, and inflammatory disease is slowed by swelling and fluid retention. Serrapeptase speeds up healing by removing scar tissue and unwanted inflammatory proteins, and by facilitating fluid drainage.
One double-blind study examined the effect of serrapeptase on post-operative swelling and pain in 66 patients who had just received surgery for repair of a ruptured lateral collateral knee ligament. On the third post-operative day, the group receiving serrapeptase exhibited 50 percent less swelling and significantly lower pain levels than controls.
Anti-microbial effect; digests biofilm; potentiates antibiotics; speeds healing from infections
Serrapeptase blocks the ability of pathogenic microorganisms to generate biofilm, the microbial secretions that form a protective wall around bacterial and fungal colonies. Serrapeptase digests this biofilm barrier, allowing immune cells and antibiotics to move in for the kill.
An alternative to NSAID drug toxicity
The July 1998 issue of The American Journal of Medicine discussed NSAID-related gastrointestinal and metabolic complications: "Conservative calculations estimate that approximately 107,000 patients are hospitalized annually for non-steroidal anti-inflammatory drug (NSAID)-related gastrointestinal (GI) complications and at least 16,500 NSAID-related deaths occur each year among arthritis patients alone. The figures of all NSAID users would be overwhelming, yet the scope of this problem is generally under-appreciated."
The usual recommended dose is 2-6 enteric-coated capsules once or twice daily on an empty stomach. (This is important because serrapeptase will digest the protein in food rather than being absorbed intact.) The total dose of serrapeptase per day is between 10 and 30 mg on an empty stomach preferably in three divided doses.
Be sure the serrapeptase product you choose comes with a pH resistant enteric coating to ensure protection from stomach acid, allowing disintegration only after entering the alkaline environment of the small intestine. This increases small intestinal absorption, thus enhancing systemic activity and efficacy.
Products vary in quality and potency. Some companies marketing deceptively-named serrapeptase knockoff products that they claim are comparable or equally effective. When considering these products and claims, keep in mind that the published research was done on serrapeptase, not the wannabes.
Do not use with blood thinners. Systemic proteases like serrapeptase have antithrombotic properties and may therefore increase clotting times in persons taking Coumadin (warfarin), aspirin, and Plavix. Patients taking antibiotics should consult a physician before taking Serrapeptase as it may improve vascular permeability, thus increasing the rate of antibiotic absorption and delivery.
An essential nutrient (like a vitamin, but oily) flaxseed oil (FSO) is a broad-spectrum anti-inflammatory agent that serves up a bonanza of heart-healthy effects: beyond strengthening the cells of the vascular wall, FSO lowers C-reactive protein, cholesterol, LDL, and fibrinogen.
FSO also lowers levels of clot-promoting thromboxanes, a family of compounds found in blood platelets (blood clotting cells). Thromboxanes encourage platelets and red blood cells to stick together, forming a clot - that's blood clot, as in heart attack or stroke. Researchers report that the alpha-linolenic acid in flaxseed oil markedly lowers the biosynthesis of unfavorable thromboxanes and fibrinogen, thus inhibiting the platelet aggregation and excessive thromboxane activity that accelerate clot formation.
1 tablespoon or 6-8 capsules daily.
This proteolytic (protein-digesting) enzyme derived from pineapple stems is one of the most effective fibrinogen-lowering agents. Bromelain (Ananas comosus) activates plasmin, our bodies' own enzyme for lowering fibrinogen levels. Activated plasmin digests both fibrinogen and fibrin.
Bromelain is a blood thinner. Therefore, individuals taking warfarin, Coumadin or other prescription blood thinners should discuss bromelain with their alternative health care practitioner before deciding to take it.
2-6 250 mg capsules two or three times daily, taken away from meals if possible).
Rich in flavonoid catechin polyphenol antioxidants such as EGCG (epigallocatechin gallate), green tea lowers fibrinogen levels and protects against cardiovascular disease. Research and 25 years of clinical use in Europe and Asia has demonstrated that green tea reduces the risk of cancer, osteoarthritis, impaired immune function, infection, gum disease, and even tooth decay.
EGCG, the main active component in green tea leaves, protects your cells from oxidative damage by those nasty omnipresent free radicals that can shorten your life by causing cancer, arteriosclerosis, heart disease and accelerated aging. EGCG inhibits oxidation of fats (including the all-important LDL particle), and assists in weight loss. The polyphenols in green tea improve blood sugar regulation in persons with insulin resistance, lower cholesterol, and block the development of the clots (called anti-thrombotic activity) that lead to heart attacks and strokes. EGCG and other green tea phenols also protect our DNA from ultraviolet and visible radiation-induced damage: at least one researcher has shown that sipping green tea before exposure decreases sunburn. Black tea leaves contain a little EGCG but much less than the green alternative.
2-4 capsules green tea extract (500 mg each providing 250 mg of catechins and polyphenols) once or twice daily, or 2-8 cups per day of organic green tea.
See Chapter 11: Blood Sugar, Insulin Resistance, and The Metabolic Syndrome.
Whip yourself up a tasty curry dish pleasantly seasoned with lots of turmeric (curcumin; curry powder), olive oil, garlic, onions, shallots and ginger. Every single one of these ingredients will contribute to a reduction of your fibrinogen level.
Shown to lower fibrinogen in humans with elevated fibrinogen levels. Use olive oil in salad dressings and for cooking as your principal source of dietary fat.
Two to four capsules once or twice daily, or cook using fresh cloves.
An anti-inflammatory herb. Better than aspirin at blocking clots. Like aspirin, ginger exerts its anticoagulant effect by inhibiting the enzyme COX-1 (which increases platelet stickiness in preparation for clot formation).
Whenever possible, cook with these fibrinogen lowering foods: garlic, ginger, onions, shallots, rosemary, and turmeric (curcumin).
Organic green (not black) tea contains numerous compounds shown to prevent and reverse damage to the cardiovascular system. In Asia, it is not unusual to drink 8-10 cups a day. (See description of green tea in supplement section above.)
The traditional cooking style of countries bordering the Mediterranean Sea, this diet has been shown in numerous large-scale studies to be associated with significantly low risk of cardiovascular disease. The Mediterranean Diet specifically lowers fibrinogen. The key components of a Mediterranean Diet include:
No FDA-approved drug will lower your fibrinogen level.
The popular cholesterol-lowering drug Lopid (gemfibrozil) actually increases fibrinogen levels by 10 to 20%!
Coumadin (warfarin) reduces the risk of clots in the short run, but is a toxic drug with multiple adverse effects, including hemorrhage, necrosis, and osteoporosis. Nattokinase is preferable because it reduces coagulation gently and naturally, and because (unlike Coumadin) it dissolves clots and thrombi that have already formed.