Superior Index Go to the next: Chapter 12
Print Files: A4 Size.
Dave Shoemaker, a fifty year old English professor at a small private college, had worked hard, played hard, loved his wife, his job, his friends, his life. He didn't want his world to change.
A football fanatic, Dave kept a San Francisco 49ers helmet signed by Joe Montana in a glass case in his study. He loved to cook, and his wife loved him for it. Together they had many friends, and an active social life. Old hippies, they regularly attended rock concerts. Deeply committed to his two teenagers, Dave stayed involved in their lives, driving them (and often whole teams) to volleyball and soccer games, donating most weekends while putting other important areas of his life on hold.
Three years ago Dr. Oakes, Dave's family physician, discovered that his blood pressure was "a little high, nothing to worry about, nothing we don't expect at your age". Noting that Dave's dad and uncle had both died of heart attacks, Dr. Oakes prescribed a diuretic to keep the blood pressure down.
Dave carried a bit of a pot belly (we call this "central adiposity"), so Dr. Oakes also suggested a weight loss program. Having followed his doctor's orders for blood pressure and weight loss, Dave felt he was "home free" and needn't fear a heart attack. Nothing could have been further from the truth.
"One cool spring evening after his typical low fat dinner, Dave's good life came to a screeching halt. He had been helping his 18-year-old, Mandy, with her homework, and, `Out of the blue I have this tight, crushing feeling, like an elephant standing on my chest,' he told the ER doctor. `I can't get my breath. Millie drove me here. What's wrong?' "
"The doc placed his hand reassuringly on Dave's right shoulder and in slow, even, comforting tones, said, `Mr. Shoemaker, you are having a myocardial infarction.' "
"That's impossible! My blood pressure is fine, my cholesterol is normal, and I've been eating a low fat diet for a very long time. Okay, I'm a little overweight, but how could I be having a heart attack?"
"Please calm down, Mr. Shoemaker. It's not good for your heart! We don't know why, but about half of all heart attack patients are like you: their blood pressure and cholesterol are normal and they eat a low fat diet. Right now, we have to worry about stabilizing you. Later on, you can talk with your family doctor about why this happened, okay?"
"Dave was admitted, and the next morning, when Dr. Oakes visited him on the ward, Dave posed the same questions."
"Dave," he replied with a shrug, "we don't know why simply lowering cholesterol and blood pressure isn't curative for so many people. It's true, you are doing everything right. It could be genetics; perhaps your family history is predisposing you to this. You just have to `learn to live with it.' " (I hate it when they say this because it's never true.)
"What neither Dave, nor Dr. Oakes, nor the ER doctor realized was that Dave suffered from a disease complex known as `the metabolic syndrome' (TMS)."
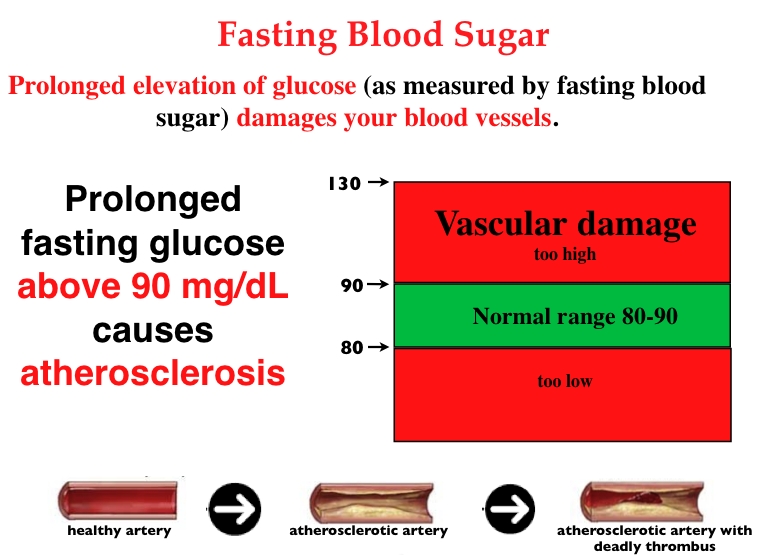
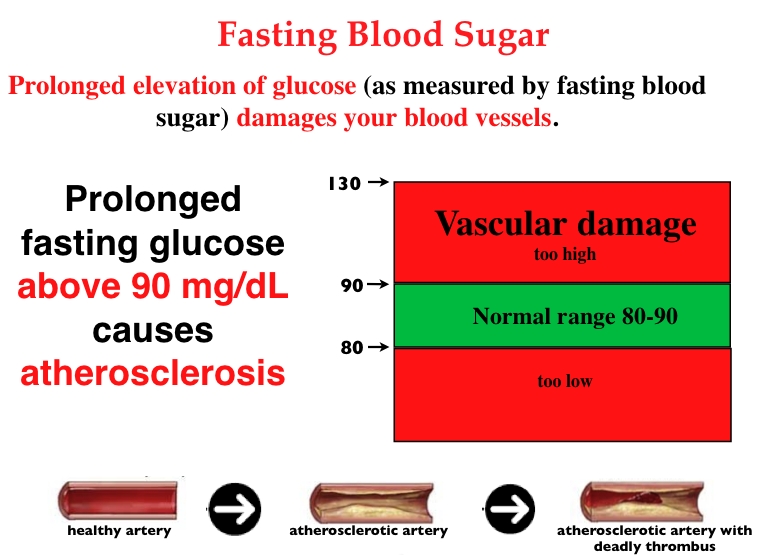
Prolonged fasting glucose, above 90 mg/dl, causes atherosclerosis.
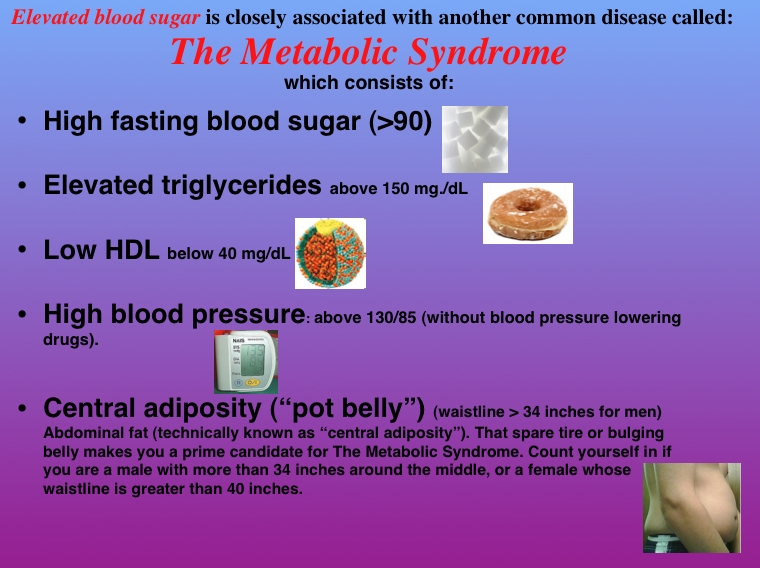
Gerald Reaven, Ph.D., of Stanford University was the first to recognize the metabolic syndrome. His research showed a statistical association between elevated blood sugar levels and four other markers: high triglycerides, low HDL, high blood pressure, and waistline expansion. Reaven originally assigned the name "Syndrome X" to this cluster of variables. Others have referred to TMS as "dyslipidemic hypertension" or "insulin resistance syndrome". Though catchy, the "Syndrome X" moniker has lost favor, gradually bowing to the more technically accurate "the metabolic syndrome".
If you have any three of the following five signs, you have the metabolic syndrome:
If you are over forty, a little overweight, have a slightly protruding abdomen (a pot belly, even a teeny one), and tend to be a couch potato, the likelihood is high that you have TMS.
One in four Americans has TMS. Most people over 50 have TMS. The risk conferred by
TMS is so high that people who have it can be thought of as working on their first heart attack.
The first sign of TMS is usually a rise in fasting blood sugar levels above 90 mg/dL. (Fasting blood sugar can be measured alone, but is also a component of the standard "comprehensive metabolic panel".)
Before Reaven's research, we knew that extra blood sugar triggers a sequence of metabolic and hormonal events that ravage the endothelium. All by itself, a persistent elevated fasting blood sugar (FBS) was known to cause accelerated atherosclerosis. But Reaven was the first to show that the already high risk of heart attack conferred by an elevated FBS becomes exponentially higher if the individual also has at least two of the remaining four factors (a "spare tire" - even a tiny one, high triglycerides, low HDL, and/or high blood pressure).
An elevated fasting blood sugar (and/or TMS) tells us that this patient has lost the ability to manage blood sugar. More specifically, he or she has developed a condition known as "insulin resistance," a metabolic disorder in which insulin receptors have stopped responding to insulin.
Here's how insulin resistance works. We need energy to drive the many chemical reactions of life and we get that energy by burning fuel (the sugar glucose) in oxygen (supplied by the lungs). We need a constant and evenly released supply of glucose. Too much or too little causes problems. The blood sugar regulating system I am about to describe makes sure the burning process is steady.
As food is absorbed after every meal, blood sugar levels rise. Your pancreas monitors blood sugar and, when it detects that rise, it secretes extra insulin into the bloodstream. When insulin arrives at the outer surface of liver and muscle cells, it attaches to insulin receptors there and sends a command telling that cell to remove excess sugar from the bloodstream and store it as glycogen for use later on. This system, when healthy, works to keep blood sugar steady.
With insulin resistance the insulin receptors have grown weary and begin to respond sluggishly to the insulin messages. The receptors appear to be "resisting" the insulin messages. When insulin resistance sets in, the muscle and liver cells remove less sugar from the bloodstream, and - since less sugar is being removed - this causes a rise in fasting blood sugar (FBS). When FBS reaches 90 mg/dL or more, we know that insulin receptors are damaged and malfunctioning.
Soon the pancreas figures out that its insulin messages aren't being heard, so it tries to fix the situation by ratcheting up insulin production. People with insulin resistance and the metabolic syndrome therefore typically have high levels of insulin in the blood ("hyperinsulinemia").
Though doctors may use a variety of terms to describe insulin resistance, including "blood sugar dysregulation," "elevated blood sugar," and "pre-diabetes," the underlying cause is always the same: loss of control over blood sugar because of damage to insulin receptors.
Insulin resistance does not happen in a vacuum; it's usually accompanied by a pattern of other signs indicating the presence of the metabolic dysfunction. The diagnosis of TMS is an attempt to incorporate a diagnostic recognition of these additional changes. As mentioned above, when insulin resistance occurs (as manifested by blood sugar > 90), it is often accompanied by four related metabolic phenomena: rising triglycerides, lower HDL level, elevated blood pressure and abdominal fat accumulation (pot belly). When doctors see these signs, they will (hopefully) recognize and treat TMS.
The diagnosis or TMS requires at least three of the following five signs:
TMS is not a rare disorder: 75 million Americans suffer from it. Like Dave, very few know they have it. Dave's blood sugar had crept up to well over 100 (as you know, anything over 90 is too much). His triglycerides (TG) were over 200 (up to 150 is okay) and his HDL (the "good" cholesterol) had dropped below 35 (should be > 40). These three markers, plus central adiposity (fat around the middle) and elevated blood pressure constitute the five cardinal signs of TMS. Dave had them all.
Dave came home from the hospital with more drugs. His TMS, however, went undiagnosed. No one told him to exercise. No one told him he had to cut way back on carbs. No one explained how to use nutritional supplements to reverse his insulin resistance. After three months on this "program," Dave suffered a second massive coronary occlusion. This time he almost died. Again, the doctors failed to make the correct diagnosis. Dave began wondering whether his treatment plan was working, and a friend referred him to me. The diagnosis of TMS was simple because he had all of the symptoms and signs of it. Once we got him going on a program for TMS (see below), he started improving.
TMS is never accompanied by any discomforting symptoms, so why would one care whether it's happening? In a word (okay, two words): accelerated atherosclerosis. Persistent blood sugar elevations damage arteries, cause plaque deposition, and accelerate the atherosclerotic changes that lead to strokes and heart attacks.
Many doctors dismiss minor elevations of fasting blood sugar. If your doctor does this, have a long talk (good luck with that; most doctors are too busy!), then show him or her this book, and if you still get resistance, it may be time to move on. Like Dave, you need a physician who understands the metabolic syndrome and knows how to treat it aggressively.
Other than a pudgy waistline (and this might not even be present), there may be no outward signs of TMS. As I have emphasized throughout this book, to detect risk one must do the biomarker testing and know the numbers.
Every year thousands of patients die because their physicians ignore the signs of TMS while overestimating the relative importance of lowering cholesterol.
If you have any three of the following five signs, you have the metabolic syndrome: extra fat around your middle, a fasting blood sugar above 90, triglyceride level over 150, HDL less than 40, high blood pressure.
Other risk markers often (but not always) found in conjunction with the metabolic syndrome include:
Poor diet, stress, smoking, alcohol consumption, and sedentary lifestyle increase risk for developing TMS.
The convergence of markers for TMS is far more ominous than an elevation of any individual heart marker, so doctors who understand cardiovascular disease take it very seriously.
Men and women with TMS constitute the group at greatest risk of death from heart attack. In fact, studies have shown that the risk of heart attack, heart disease, and stroke is nearly three times higher in people with the metabolic syndrome. According to Dr. Steven Nissen, distinguished Cleveland Clinic cardiologist, "This is the disease of the new millennium".
The Centers for Disease Control (CDC) tells us that one in four adults in the U.S. (about 75 million individuals) has signs of metabolic syndrome and will most likely die from it.
The numbers are expected to grow because of Americans' sedentary lifestyle. A study of 1,209 men aged 42 to 60, over a 15-year period, found that those with metabolic syndrome were from 2.9 to 4.2 times more likely to die of a heart attack than those who did not have the condition.
"I see now, patients in their 20s and 30s with the metabolic syndrome and this does not bode well for their risk of heart attack and stroke when they [reach] 40 or 50 years of age," says Richard Nesto, M.D., Associate Professor of Medicine, Harvard Medical School, and Chairman of the Department of Cardiovascular Medicine at Lahey Clinic (a teaching hospital of Tufts University).
"The metabolic syndrome has been there for a while," says Dr. Nesto. "We just have not recognized its importance. I think doctors in the past have looked at patients without looking at the big picture," he said. "They've looked at risk factors in isolation and treated them one by one. Now we should look at patients as to whether they have the metabolic syndrome."
If one examines the individual risk factors separately, they don't seem all that bad. When taken together, however, you end up with a skyrocketing atherogenic potential that is far greater than just the sum of the parts. Doctors can no longer afford to isolate and treat individual risk factors such as cholesterol or hypertension. This was the approach Dave Shoemaker received, and it produced a disaster.
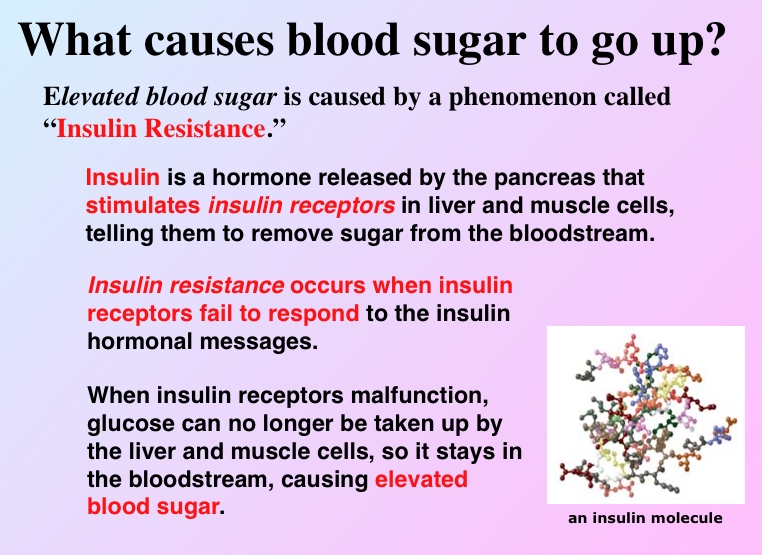
Elevated blood sugar is caused by a phenomenon called "Insulin Resistance".
"Insulin is a hormone released by the pancreas that stimulates insulin receptors in liver and muscle cells, telling them to remove sugar from the bloodstream."
"Insulin resistance occurs when insulin receptors fail to respond to the insulin hormonal messages."
"When insulin receptors malfunction, glucose can no longer be taken up by the liver and muscle cells, so it stays in the bloodstream, causing elevated blood sugar."
Okay, now you know what to look for - and why it's important. You already know that the main causative factor for the metabolic syndrome is insulin resistance, caused when insulin receptors fail and blood sugar climbs. Now I am going to take you a little deeper into the biochemistry and molecular biology of it.
Let's start with how blood sugar is regulated in a healthy body. The food we ingest contains carbohydrates which are digested down into sugars that are then absorbed into the bloodstream. These absorbed sugars raise our blood sugar (glucose) level. Our pancreas detects this rise in blood sugar, and secretes a little extra insulin, which travels through the bloodstream to the liver and muscles. There it attaches to insulin receptors on the surface of liver and muscle cells, telling them to remove some of the sugar from the bloodstream (to be stored as glycogen for later use). Removal of some sugar lowers the blood sugar level, so the pancreas decreases its insulin production.
There's a feedback loop here. The liver and muscles are continuously "listening" to the insulin "messages" sent from the pancreas, and removing more sugar if the "volume" goes up. The pancreas is likewise "listening" to the blood sugar level; it increases insulin production when the sugar goes up and decreases it when sugar goes down.
Now imagine what would happen if the insulin receptors in the liver and muscles began turning a deaf ear to the insulin. First you'd have less sugar being pulled out of the bloodstream and stored as glycogen. Then blood sugar levels would rise. The pancreas would notice this and compensate by releasing more insulin. That insulin would not be completely effective at clearing the extra sugar, so the pancreas would work harder to make and more insulin, but less and less of the sugar would be removed, so the blood sugar would creep higher. Once it's consistently above 90, insulin resistance is born - and along with it, accelerated atherosclerosis.
If insulin receptor failure persists, the blood sugar can go even higher. If it reaches 115, we now have full-blown type 2 diabetes, but more often it hangs out in the 90-110 range-clear-cut TMS. Either way, there is a problem.
Why do insulin receptors fail? We don't know, but we do know that its appearance is almost always accompanied by some combination of excess carbohydrate consumption, insufficient exercise, aging (it's way less likely in people under 40), and genetic predisposition.
TMS develops slowly, and a decade or so may pass during which slight abnormalities in blood sugar, blood pressure, triglycerides, abdominal fat and HDL go unnoticed. Watch for this "upward creep," and if your belly is bulging a little or your blood pressure is higher than it had been, get tested. If your triglycerides and blood sugar are slipping upwards or your HDL downwards - even though they may still be in the normal range - this is probably TMS in the making. Diagnosing your own TMS and reversing it in the earliest stages is far preferable to waiting until a doctor diagnoses it in the advanced stages.
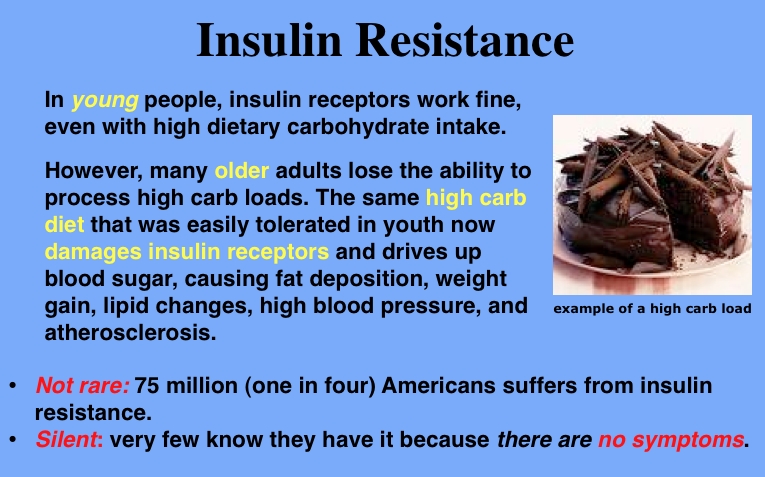
In young people, insulin receptors work fine, even with high dietary carbohydrate intake.
However, many older adults lose the ability to process high carb loads. The same high carb diet that was easily tolerated in youth now damages insulin receptors and drives up blood sugar, causing fat deposition, weight gain, lipid changes, high blood pressure, and atherosclerosis.
It is important to know that you have control over your TMS; you can reverse it. There are three main causes of TMS: sedentary lifestyle, high carb diet, and aging. There isn't much any of us can do about getting older, but you can exercise every day, and you can choose to eat a low carb diet. That's enough to normalize blood sugar in most individuals.
We live in the midst of an epidemic of excess carb intake that causes insulin overload that, in turn, causes obesity. Eating too many carbohydrates has some very undesirable consequences. First, our pancreas secretes excess insulin in an attempt to remove the extra sugar from the bloodstream and store it (as glycogen) in the liver and muscles. When the liver and muscle stores are full (it doesn't take much), the body still has to do something with remaining blood sugar, so guess where it goes? It's converted to fat and that fat is stored in the belly. The excess insulin that's stimulated by excess carbohydrates ends up promoting the accumulation of body fat. Therein lies a big (pun intended) problem: central adiposity, or fat around the middle. Lowering carb intake reverses this process, and reverses insulin resistance and TMS at the same time.
Exercise is the first line of treatment for metabolic syndrome because it influences all components of the disorder. Regular physical activity helps reduce excess body fat. Exercise improves insulin sensitivity. Exercise helps normalize blood pressure, as well, especially in people with borderline hypertension, the type of hypertension seen in metabolic syndrome. Exercise raises HDL cholesterol levels.
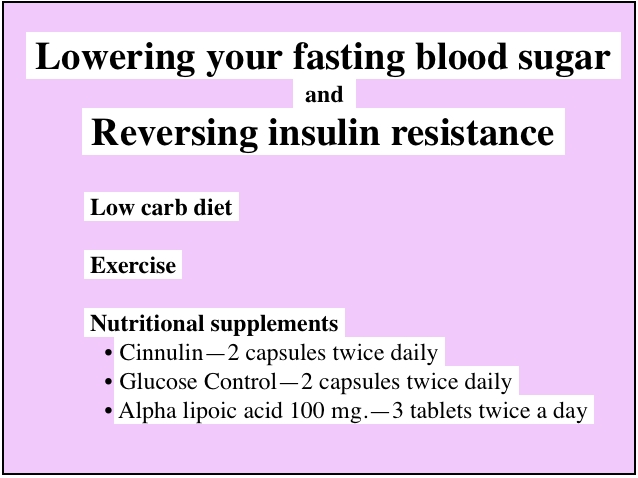
Diet, exercise, and nutritional supplements are the three pillars of therapy for the metabolic syndrome. When it comes to treating TMS, mainstream and alternative doctors agree that the starting point is always diet and exercise. Specifically, a low carbohydrate diet and one hour of daily vigorous (i.e., aerobic) exercise will usually correct insulin resistance and reverse the metabolic syndrome. (If you need to lose weight, make that one and a half hours daily.) Both components, diet and exercise, are absolutely necessary.
The addition of Cinnulin®, Glucose Control, and alpha lipoic acid will accelerate your progress by supporting the healing of insulin receptors.
Your program will need to address all components of TMS. So - if your triglycerides are elevated, your HDL low, your BP elevated, or waistline bulging - these must also be addressed as well. The diet and exercise prescription will go a long way toward correcting all of these. See recommendations below and in the corresponding chapters for additional advice.
Experts agree that shifting to a low carbohydrate diet is essential for reversing insulin resistance and curing the metabolic syndrome. It's a common misconception that low carb dieting has to be painful.
Pay attention to carb levels in food types:
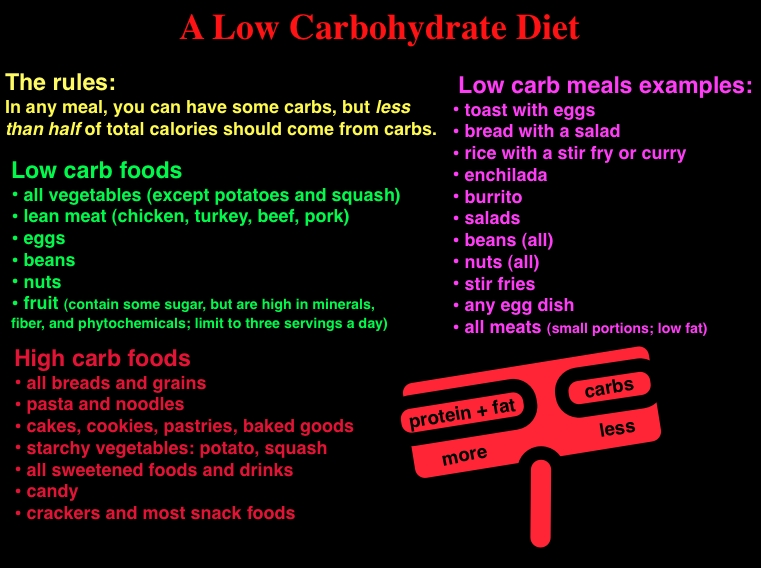
Keep in mind what I call "The Golden Rule of Low Carb Dieting." In any given meal, fat calories plus protein calories must be greater than carbohydrate calories. Know carb food contents as listed above and read labels. Learn to quickly "eyeball" the carb content of a meal or snack. The "Golden Rule" makes it easy. Examples of low carb meals: eggs and toast, a chicken sandwich, salads, nuts with dried fruit, meat and vegetables. Just follow these simple guidelines:
Read labels on packaged foods to determine carb content.
This may seem tedious at first, but once you get to know the carb content of your favorite foods, it will get quicker and easier.
It is impossible to reverse the metabolic syndrome without a daily exercise program: it's the sine qua non for success.
I am not talking here about climbing the stairs or parking your car and walking a few extra blocks to work (though not a bad idea). This exercise program consists of daily one hour workouts divided more or less equally between aerobic and strength components. If you need to lose weight, make that 1.5 hours.
If you have never been on an exercise program, enlist the services of a qualified trainer who can get you going on a custom-tailored program. It is absolutely crucial that you start out at a low level and increase very gradually. Having watched many patients initiate exercise programs in my 40 years of medical practice, I can tell you that it is an absolute certainty that you will suffer a potentially disabling injury if you increase your activity level too rapidly. Go slow at first and work up gradually!!! Your body needs time to get used to increased exercise, and if you push up your level too fast, you'll injure yourself. Going slow doesn't mean devoting less time; it just means going slower at first. Pain and excess fatigue are the two most common warning signs of over-exercising.
Most of us are so busy these days that we balk at the notion of yet another demand on our time. Can you afford an hour a day out of your already over stressed schedule? How important is it? Only you can answer these questions. But I would argue that finding the time - making it a priority - is an ultimately practical thing to do. Your investment in exercise time will pay huge dividends "down the road," as it were - a stronger body and a longer and healthier life, devoid of the heart attack, stroke, hospitalization, debility, high health care costs, and a very much higher risk of premature death. Not to mention more time with the grandkids.
Why does exercise work? It improves our biochemistry and physiology in so many ways that I can only begin to explain it. Daily workouts widen and lengthen the freeway system of your blood vessels, and this enhances your body's ability to deliver nutrients and fuel to all 100 trillion (or so) of your cells. By strengthening the heart muscle and building collateral vessels, exercise develops those alternate routes that come in real handy if one of the main freeways - like, perhaps a coronary artery - becomes blocked. Because "widened freeways" can remove waste material far more efficiently, conditioning is one of the most effective detox secrets around. In a physically fit individual, more blood (carrying more nutrients and oxygen) is delivered to even the most remote regions of your body. These are tissues that would otherwise be struggling and competing for supplies: the brain, liver, kidneys, immune system, sense organs, sex organs, endocrine glands - all start functioning better because they are no longer in a state of chronic semi-starvation.
Exercise addresses all five components of the metabolic syndrome: it reduces body fat, controls glucose levels by improving cellular insulin sensitivity and responsiveness, increases the ability of insulin receptors to bind with insulin and remove glucose from the blood, raises HDL levels, and normalizes blood pressure.
If exercise were available as a pill it would be the strongest known medicine - by a country mile.
Dr. Richard A. Anderson and his colleagues at the Beltsville Human Nutrition Research Center of the U.S. Department of Agriculture screened extracts of 49 culinary and medicinal plants in a search for one that could mimic the effects of insulin, the hormone that regulates our blood sugar levels. They discovered that an extract of cinnamon acted like insulin in human cells. The active component in cinnamon responsible for its insulin-like activity is a water-soluble chemical compound called methylhydroxychalcone polymer (MHCP). They further found, to their amazement, that MHCP delivered insulin activity identical to insulin. In other words, insulin receptors were unable to distinguish the difference between MHCP and insulin. The cinnamon-derived compound did exactly what insulin does: it occupied insulin receptors in the liver and muscles and ordered them to remove glucose from the bloodstream and store it as glycogen. The cinnamon not only mimicked insulin, it enhanced insulin receptor sensitivity to insulin. They showed that insulin plus MHCP provided an effect that was greater than the sum of the parts. Taken over a period of several months, MHCP helped insulin receptors to heal.
When cinnamon extract (Cinnulin®) was given to human patients who had insulin resistance, the results were dramatic. After 40 days of treatment, blood sugar levels were reduced by 18-29%. This means that an insulin resistant patient (e.g., type 2 diabetes or metabolic syndrome) with an average blood sugar level of 120 could expect reductions down into the normal range (80-90) simply by taking MHCP cinnamon.

Whole cinnamon is not recommended as it contains naturally-occurring coumarin, which has activity similar to the commonly-used blood thinning drug, Coumadin. Consuming large quantities of supermarket cinnamon on a regular basis might therefore pose a health risk, especially for individuals taking blood thinners. Coumarin is removed from quality cinnamon extract products marketed as "Cinnulin®" nutritional medicinals.
Cinnulin® cinnamon extract will also reduce blood lipids. The MHCP in it has been shown to reduce total cholesterol, LDL cholesterol, and triglycerides.
I've noticed plain cinnamon spice in capsules in certain chain drugstores. Steer clear of these products; there's no reason to believe they'd work.
Dose: 125 mg per capsule; take 2 capsules twice daily. (Do not use unprocessed supermarket cinnamon.)
Alpha lipoic acid (ALA), a powerful broad-spectrum antioxidant, reverses insulin resistance and supports several other critical aspects of heart health. ALA protects the endothelium, reduces oxidative stress, and recycles other heart protective antioxidants (especially vitamins C and E).
Dose: Supplied as 100 mg tablets. Take 200-1200 mg per day.
This combination of nutritional medicines reverses insulin resistance by bolstering the body's sugar management systems:
Dose: Renewal Research Glucose Control. 1-2 capsules twice daily;
Take 200-1000 mcg/day. (Or take Glucose Control.)
(Barlean's brand) - one tablespoon or 6 caps daily
Lowering your triglycerides lowers blood sugar
See complete triglyceride lowering program in Chapter 7.
If your blood pressure is elevated (above 130/85), your first line of treatment should be exercise. In 85% of people with mild to moderate hypertension, exercise alone is curative. In most cases, daily exercise, a low carb diet, and weight loss will gradually lower blood pressure into the normal range without the need to resort to drugs. I've already described the kind of exercise program this requires.
If you've given it an adequate trial (one hour of aerobic exercise a day for two months) and exercise alone truly does not work, continue the exercise program, and add nattokinase (see Chapter 10 for details).
If, after two months, your blood pressure is still elevated, ask your doctor to start you on hydrochlorothiazide, a gentle diuretic that is generally well tolerated. (Many antihypertensive drugs are toxic, so avoid them unless absolutely necessary.)
Keep in mind that a diet rich in fresh fruit and vegetables will go a long way toward controlling hypertension.
The abdominal fat deposits (less sensitively known as "pot belly") that characterize TMS will melt away naturally when you follow the low carb diet and daily exercise program described above.
Now let's take a look at how the size of your LDL particles dramatically influences cardiovascular risk ...