Superior Index Go to the next: Chapter 8
Print Files: A4 Size.
Everything we eat is composed of just three types of nutrients: fat, protein, and carbohydrate. The proteins (digested down into individual amino acids) and the carbohydrates (digested down into individual sugar molecules) are soluble in water, and so can be easily shipped through the bloodstream. Fats, on the other hand, are not water soluble, so Nature had to find a way to package up in order to ship them around in the body. Lipoproteins, specialized water-soluble particles that enable lipid transport, are the "solution" to this problem. Synthesized in the liver, lipoproteins solubilize lipids, ferry them about to the far reaches of the body, and then unload them at specific target sites.
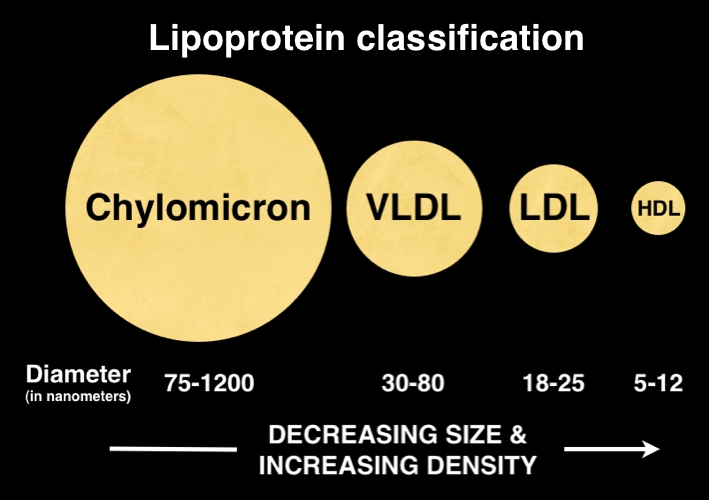
Though there are many types of lipoproteins, the three most important ones are found on a standard lipid panel: LDL, HDL, and VLDL.
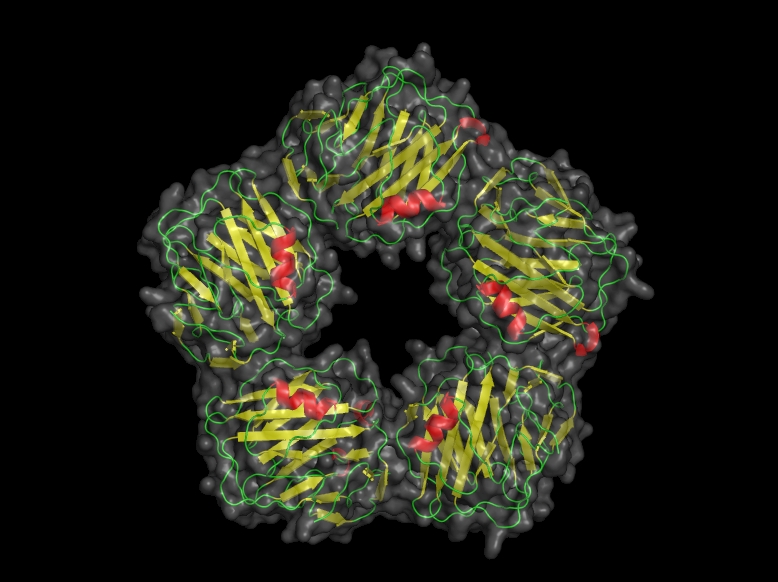
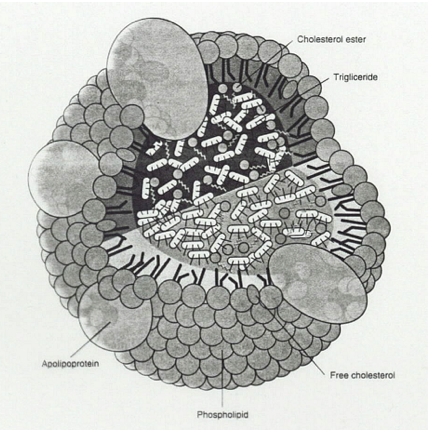
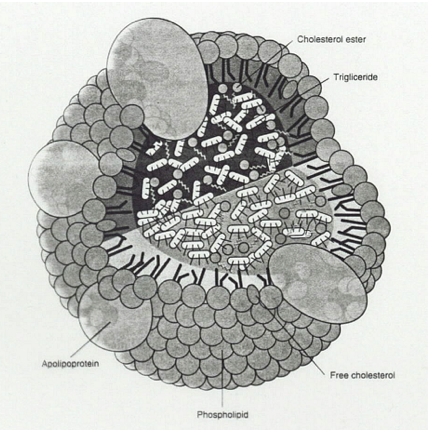
Lipoproteins are tiny, nanoscale balls whose outer wall is a single layer of fat (phospholipids and cholesterol) with protein molecules embedded in it. The inner contents - the payload, if you will - of lipoproteins includes cholesterol, triglycerides, and small amounts of other lipids.
Lipoproteins come in a variety of sizes, ranging from very small to very large. Of course my use of the word "large" here is relative; all lipoproteins are tiny. We measure their size in nanometers (nm), or billionths of a meter.
HDL (high density lipoprotein) particles are the smallest lipoproteins. They range from 5-12 nm in diameter. LDL particles are somewhat larger, averaging 18-25 nm, and VLDL (very low density lipoproteins) are the largest of all, averaging 30-80 nm in diameter.
If an HDL particle were the size of a softball, LDL particles would be the size of a soccer ball and VLDLs would be the size of a beach ball. The triglycerides carried around inside these lipoprotein particles would be marble-sized and the cholesterol molecules would be the size of a pea.
In the following sections I'll discuss each component of the Lipid Panel. And if your numbers are off, you'll learn how to fix them.
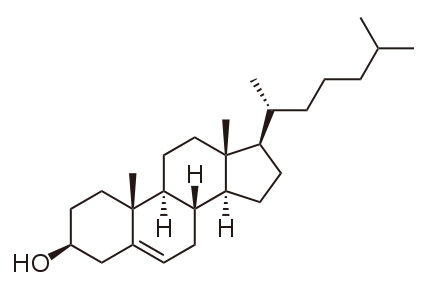
What's the first thing you think of when you hear the word "cholesterol"? Most folks associate the word with disappointing outcomes: heart attacks, strokes, hardening of the arteries, bypass surgery. It might surprise you to learn that cholesterol is actually a good guy, a steroid-type molecule that is crucial to our existence. Without cholesterol, life as we know it would be impossible. So allow me to tell you a little more about cholesterol, a molecule no less necessary for optimum health than vitamin C and insulin.
Synthesized in the liver and most other body tissues, cholesterol is a relatively simple molecular building block used by our bodies to manufacture hundreds of other molecules.
Cholesterol is a crucial structural component of the walls that surround every one of your 100 or so trillion cells.
We'd be hard put to reproduce our species without the estrogen, progesterone, testosterone, and hundreds of other steroid hormones manufactured from cholesterol in our ovaries and testes.
In the adrenal glands, cholesterol is the starting point for synthesis of over 150 stress management hormones (including pregnenolone, DHEA, cortisol, etc.). These steroids manage stress and inflammation (for example, allergies, infections, trauma) and immune responsiveness.
The liver transforms cholesterol into bile juices that are delivered to the intestinal tract to digest and absorb fats. Without this form of cholesterol, we would be unable to absorb the essential fatty acids and fat soluble vitamins (A, D, E, and K) from food and supplements.
In the skin, ultraviolet light transforms cholesterol into vitamin D (which is also a hormone). Recent research has shown vitamin D to be far more important than we originally imagined. Beyond its role in calcium metabolism and bone health, D is now known to play critical roles in mental health, blood sugar regulation, immune health and cancer prevention.
Without cholesterol, we'd be in big trouble: we'd have no protection from stress, no sex life, nothing to keep our cells from falling apart, our risk of degenerative disease would skyrocket, cancer would be far more prevalent, and we'd die young. So cholesterol can't be all bad.
If cholesterol does so many good things, why does it have such a lousy reputation? Let's face it: elevated cholesterol is intimately associated with high risk of heart attack and stroke, so most people think of it as a kind of molecular mass murderer. Millions of human deaths every year can be traced directly back to elevated blood levels of this waxy molecule. How could a substance so important to our well-being have gone so far astray? To answer this question, you need to know a little more about cholesterol and LDL, its partner in crime.
There are only two ways cholesterol can get into your body (and from there into the bloodstream and perhaps deposited as plaque in the walls of your arteries):
First let's consider the outside sources - the dietary sources - of cholesterol. The amount of cholesterol we eat is determined solely by the amount of animal food we consume. All animal foods (seafood, beef, poultry, eggs, dairy) contain cholesterol. No plant food (fruit, vegetables, grains, beans, nuts, seeds) contains cholesterol. So those who choose to eat vegetarian are automatically on a cholesterol-free diet.
The amount of cholesterol we make is genetically determined, and varies greatly from one person to the next. That's why some people - the ones who are programmed not to make much cholesterol - can easily lower their blood level by simply reducing the amount of cholesterol-laden animal foods they eat. Dietary restriction works for this group because their extra cholesterol is all coming from diet.
Others, however - and I am a card-carrying member of this group - are genetically programmed to make lots of cholesterol, regardless of how much we consume. We find it impossible to lower our cholesterol by simply restricting animal foods. Even if we eat a vegan (cholesterol free) diet, our bodies just ramp up the cholesterol-manufacturing machinery to make up for the shortfall. In my case (and I am definitely not alone), without treatment, my cholesterol stays at the same high level - regardless of whether I eat vegan.
Many years ago so I tried a little experiment on myself. For one month I ate a high animal fat diet. We are talking eggs with butter for breakfast, burgers for lunch and ham or steak or chicken for dinner. Then I checked my cholesterol and it was very high at 305 (normal is less than 200). For the next month, I switched to a strict vegan diet that contained no animal foods and thus no cholesterol. If cholesterol was present, my body had to be making all of it. The lipid panel at the end of the second month was exactly the same as the one at the end of the first: 305!
My experiment demonstrated that for members of the genetically predisposed high-cholesterol group (like me), dietary cholesterol restriction (that is, avoiding animal fats) won't work. We need a more stringent program that includes the following:
When a cell needs some cholesterol (remember that all cells need cholesterol and it serves many functions in the body), that cell's DNA synthesizes LDL receptor proteins that migrate to the outer cell membrane and become embedded in it, causing the formation of a small receptor "pit". The LDL receptor then sends out signals that entice nearby LDL particles, and when one gets close, the receptor snares it. The receptor protein, along with its cholesterol-laden LDL particle, then forms a small vesicle that moves to the interior of the cell and merges with another membrane-bound sack called a lysosome. The lysosome secretes enzymes that separate the cholesterol from the LDL particle. The cholesterol is released into the cell and the LDL receptors are recycled back to the outer cell membrane where they latch onto another LDL particle and repeat the process.
Unlike all the other markers described in this book, cholesterol is an "innocent bystander," the molecular guy who happens to be in the wrong place at the wrong time. Let me explain. Because LDLs contain cholesterol, their numbers go up and down in tandem. Too many LDLs will therefore always translate into too much cholesterol. Cholesterol does not by itself cause vascular disease. It just happens to be inside of the LDL particles that (when oxidized and then devoured by macrophages) end up trapped in plaque in the walls of arteries. (For a more complete explanation of this process, see Chapter 5: Atherogenesis.)
LDLs are lipoprotein particles that function like miniature trucks. Their payload is cholesterol. Each LDL particle packs about a thousand cholesterol molecules inside its greasy outer coating and carries them from the liver to various locations around the body. Once delivered, the cholesterol is dropped off and converted into the array of biochemicals listed above: hormones, cell walls, digestive juices, vitamin D, etc.
Evidence from a very large body of research supports the notion of a close relationship between heart attacks and an elevated LDL level. Of thousands of studies, perhaps the best-known and most convincing is the Framingham long-term population study of heart disease risk, which tracked medical data and habits (dietary, exercise, smoking, etc.) of thousands of citizens of a small Massachusetts community for over five decades. Specifically, the Framingham study showed that people with elevated cholesterol levels experienced more heart attacks. This population study correlates tightly with basic science research showing that animals with experimentally induced high cholesterol levels develop atherosclerotic lesions indistinguishable from those found in humans. So, there's really no need to question that cholesterol is the bad guy, right? Well, not so fast ...
It turns out that the true villain isn't cholesterol, or even LDL. It is LDL oxidation. LDL particles in their unoxidized form present no danger to our arteries. If the LDL becomes oxidized, however, trouble is brewing. LDL particles can easily become oxidized in people with an excess of free radicals (too much junk and processed food, pesticides, pollutants, toxins, etc.) or those with a deficiency of antioxidants.
In the oxidized state, LDL has become a free radical that damages (again, by oxidation) that delicate inner arterial lining, the endothelium (see Chapter 4). Having caused local endothelial irritation and inflammation, the oxidized LDL particle can now find its way through and beneath the endothelium. Once there, it can't get out, so it accumulates, and this accumulation eventually becomes what we know as atherosclerotic plaque.
So it's oxidized LDL - not cholesterol - that's responsible for the millions of deaths every year from heart and cardiovascular disease. For decades now we have been looking at the cholesterol "innocent bystander" rather than at oxidized LDL. Cholesterol served as an adequate marker because it tracks LDL and LDL, in turn, is directly proportional to oxidized LDL. Oxidized LDL alone, however, provides a far more accurate marker for predicting cardiovascular "events". Unfortunately, oxidized LDL testing is currently not available, but hopefully that will change as increasing numbers of doctors and researchers come to appreciate its powerful causative role.
Now it becomes clear why cholesterol and LDL are weak markers. The people with high LDL and high cholesterol who never have a heart attack are the ones with lower levels of oxidized LDL.
Recent studies have shown that LDL particle size correlates with atherosclerosis progression far better than the actual number of LDL particles. Smaller, denser LDL particles are dangerous because they can more easily squeeze between endothelial cells and gain access to the wall of the artery, where they cause plaque formation. Larger LDLs can't get through, so they are associated with a great degree of safety. High concentrations of small LDL particles are associated with higher rates of cardiovascular events (heart attacks and strokes), faster progression of atherosclerosis, and higher risk of death. Conversely, high levels of large, buoyant, "fluffy" LDL particles confers great protection. See Chapter 12 for more about LDL density.
Recently formed plaque is a waxy deposit that causes a bulge on the inside wall of a blood vessel. Plaque is an inflammatory process that is going through the initial stages of healing. Like a pimple or a boil, this early plaque lesion is covered by a scab-like affair: a very thin, fragile layer of skin, below which lies a seething cauldron of cholesterol-laden gunk. If this "unstable" covering ruptures, the contents will be released and a clot will form inside the artery at the location of the rupture that can block the flow of blood through the artery. Equally devastating, the clot can form and then break loose from its moorings on the inner arterial wall, travel a short distance, and lodge downstream where the vessel narrows. This causes an "infarction".
Blockage of downstream flow in the vessel unleashes the horrific cascading sequence of events we call a heart attack: oxygen deprivation in the tissues served by the vessel, chest pain, shortness of breath, collapse, resuscitation, the risk of sudden death, ambulances, emergency rooms teeming with excellent highly skilled and dedicated workers hell bent on saving another life, intravenous clot busting drugs, pain relievers (usually morphine), hospitalization, cardiologists, get-well cards. And - in about half of all cases - a funeral.
Atherosclerotic plaque itself is not so dangerous, but unstable plaque is. We used to think that the most dangerous plaques were the largest ones, but now we know that the older, well-established plaques - because they slow the flow of blood - are the most likely to cause angina (chest pain), but are not closely associated with heart attacks. It's the small new plaques that haven't yet healed over - the "unstable" ones - that cause heart attacks.
A normal healthy person has no more than two grams of cholesterol per liter of plasma. We measure cholesterol in tenths of a liter (or deciliters), so that comes to a little less than 200 mg per deciliter. As the level rises above 200, so does risk. By the time serum cholesterol has reached 260 mg/dL the chances of a heart attack have risen to 500%, or five times the risk of a person with a level below 200.
A healthy LDL level is below 90 mg per deciliter. LDL rises with cholesterol, so when cholesterol is elevated, so is LDL.
No expert seriously questions the fact that lowering cholesterol slows, stops, and may even reverse plaque buildup and heart attack risk. However, experts most definitely do differ as to the best means to achieve this end. No doctor, alternative or mainstream, questions the value of severely restricting animal fat. Mainstream doctors, however, are smitten with the statin drug approach - but this has some serious drawbacks. Statin drugs routinely cause unwanted side effects such as muscle damage (statin-induced myopathy), liver damage, and statin-associated dementia. (Important brain structures are made of cholesterol and in some unfortunate individuals statin drugs interfere with proper brain cell metabolism.) These problems, though widely ignored and/or pooh-poohed by mainstream practitioners, are well-documented in the scientific literature. Ex-astronaut Duane Graveline, M.D., in his book "Lipitor: Thief of Memory", recounts the horrifying story of his own statin-induced global amnesia, and elucidates the many problems caused by these drugs.
The good news is that we have natural alternatives to statins that are just as effective but don't cause unwanted side effects and toxic reactions. Red rice yeast extract, pomegranate juice, and serrapeptase are among the many natural choices that lower cholesterol without toxicity. (See end of this chapter for all the treatment options.)
Lowering blood cholesterol (and with it, LDL) provides two distinct benefits. First, if there is less cholesterol to get trapped in plaque, overall plaque size will be smaller. Second, lowering cholesterol increases plaque stability - that is, it decreases the chances that unstable plaque will rupture, causing a heart attack. Even people who have already had a heart attack can substantially reduce the risk of a repeat simply by cholesterol reduction. But please: do it naturally!
Lowering your elevated cholesterol and LDL dishes out some impressive benefits. One major study followed for five years 4400 patients who had already had heart attacks. The only intervention in these patients was aggressive lowering of their cholesterol. The authors concluded that if a typical practitioner simply lowered cholesterol in his or her patients, after five years:
Clearly, cholesterol reduction works. If we take a closer look at the same data, however, another story emerges - one that underscores lipid panel limitations and the importance of comprehensive testing. In the five years of this study, almost half of these patients had a negative outcome. For every 1000 patients:
Overwhelming evidence tells us that LDL and cholesterol are bad actors. There is no question that if your cholesterol level exceeds 200, you need to get it down. However, our national fixation on cholesterol has pushed aside more important markers. Millions of lives have been lost due to this costly mistake. Cholesterol and all the other markers are "independent" of one another. This means that each - without any help from the others - can cause atherosclerosis. Testing just for cholesterol (the lipid panel) just won't cut it anymore: we need to measure and treat them all.
Why the cholesterol fixation? Why do most doctors refuse to test and treat for other, more accurate markers? One reason is that drugs provide the illusion of an easy fix. All the physician has to do is whip out his or her prescription pad and lower his patient's cholesterol. There's no statin, however - no quick and easy drug fix - for the remaining markers. Even though they all contribute to the disease process, only their weakest and least relevant member, cholesterol, gets addressed. No wonder so many people with normal cholesterol levels have heart attacks!
The problem comes down to cash flow. Nutritional supplements, exercise, and dietary changes don't generate income for Big Pharma. Massive numbers of people are dying of a preventable disease, but the industry assigned to treat it is motivated by profits. Patient welfare takes a back seat. Atherosclerotic disease is preventable and reversible, but until our health care industry develops a genuine desire to address and cure the underlying causes of this epidemic, it will continue.
Red yeast rice extract - "Nature's statin" - Take 1-2 600 mg. capsules twice daily. Used in Chinese Traditional Medicine for over a thousand years, red yeast rice extract consists of naturally-occurring medicinal compounds that regulate lipid levels without the dangers associated with statin drugs. Used to cure heart disease and circulatory disorders since the Tang Dynasty (800 A.D.), this potent herbal lowers cholesterol, triglyceride and low-density lipoprotein (LDL) levels. Contains heart-friendly phytonutrients that go far beyond simply lowering cholesterol to provide a broad spectrum of cardiovascular benefits. Red yeast rice lowers Coenzyme Q-10, so add 50 mg. a day of Coenzyme QH daily.
Pomegranate juice - Drink 6-8 ounces of pure juice daily. Lowers cholesterol and LDL, reverses atherosclerosis, melts away advanced plaque while reducing LDL oxidation. Pomegranate juice is the most powerful fruit-derived antioxidant. Must be pure organic - i.e., made from whole whole fresh fruit, no other ingredients, no other juices, no additives, not from concentrate. Use Lakewood brand "Pure Pomegranate".
Curcumin (a component of the spice turmeric) - 2-8 500 mg. phytosome capsules twice daily, or use turmeric liberally in cooking. 2-8 grams a day have been used in research studies. Lowers cholesterol and LDL and reverses atherosclerosis. Stick with Meriva® "phytosome" products in which curcumin has been bonded to a fat soluble substrate (phosphatidylcholine) to enhance absorption.
Green Tea Extract - 1-2 capsules twice daily. Green tea reduces cholesterol and LDL by increasing LDL receptor expression (as measured by LDL receptor binding activity) in the liver. Upregulating the LDL receptor reduces cholesterol by 30%.
Lower cholesterol to ideal level of 170-200 mg/dL
Lower LDL to ideal level of 70-90 mg/dL
The four most effective nutritional supplements for lowering cholesterol and LDL are red yeast rice extract, pomegranate juice (organic Lakewood PURE Pomegranate) , curcumin (as Inflammation Control), and green tea extract. These food-derived, phytochemicals should be the starting point for your cholesterol-lowering program.
Curcumin - (2-8 500 mg capsules twice daily, or use turmeric liberally in cooking.) 2-8 grams a day have been used in research studies. Though it prevents and reverses atherosclerosis via numerous mechanisms, curcumin is not well-absorbed. Purchase only "phytosome" products in which curcumin has been bonded to a fat soluble substrate like phosphatidylcholine to enhance absorption.
Green tea extract (1-2 capsules twice daily).
Garlic capsules (1-3 once or twice a day).
Low-carb, low-fat diet that minimizes animal foods (meat, eggs, dairy). Minimal amounts of extremely lean meat. Eat lots of veggies, beans, fruit, nuts and seeds.
Take 1-2 600 mg capsules twice daily.
Used in Chinese Traditional Medicine for over a thousand years, red yeast rice extract (Hong Qu) is the original herbal statin drug. This medicinal herb is just as effective as its modern drug knockoffs, but isn't plagued by the host of dangerous side effects that accompany the use of statin drugs.
As described in the ancient Chinese pharmacopoeia, Ben Cao Gang Mu-Dan Shi Bu Yi, published during the Ming Dynasty (1368-1644), the use of red yeast rice in China to cure heart disease and circulatory disorders was first documented in the Tang Dynasty (800 A.D.) and has been used ever since.
Red yeast rice is made by fermenting rice with Monascus purpureus, a type of red yeast. (Red yeast rice extract does not contain any yeast, however.) In the 1950s modern drug researchers, recognizing the potential medical importance of red yeast rice extract, but realizing they couldn't make a profit selling a non-patentable Chinese herb, stripped out the single most effective molecule (discarding the crucial supporting components), and then synthesized it. The result was the original statin drug: lovastatin (Mevacor). Unlike the Chinese herb, the synthesized drug causes severe musculoskeletal symptoms and brain damage.
Plant medicinals (herbs) contain a spectrum of active ingredients. Isolating and purifying one patentable molecule, while tossing out the other members of the family of beneficial compounds, is a prescription for side effects and toxicity. Statins are no exception. Statins, the drug version of red yeast rice extract, commonly cause severe musculoskeletal symptoms, including muscle cramping, rhabdomyolysis (breakdown of muscle tissue), myositis (inflammation in the muscle), and myalgia (pain in muscles). These symptoms are usually missed by the prescribing physician, who chalks them up to muscular misuse or old age. These adverse reactions are not seen in patients using red yeast rice extract.
The most ominous adverse reaction, however, is statin-associated dementia. This syndrome has been documented by several research reports in the scientific literature, and thousands of anecdotal reports. The "statin effect study," where patients on statins self-report side effects, tells us that 48% of patients on statin drugs report some degree of mental impairment. Statin-associated memory loss, difficulty concentrating, cognitive impairment, and either global or partial amnesia are the dark side of statins.
One of my patients comes to mind. Millie had been misplacing her keys, losing track of what she was doing, becoming easily confused. I told her about statin-associated dementia, and suggested she try going off her statin for a while. Within a week her brain started functioning again and all her symptoms went away. When Millie told her cardiologist what she had done, he fussed and fumed, called it balderdash and horsefeathers, and insisted she get back on her statin drug. Millie complied, but within a week, her cognitive and memory problems had returned in full force. She quit again, this time for good.
I recommend red yeast rice extract to my patients because it very effectively lowers cholesterol, triglyceride and low-density lipoprotein (LDL) levels and provides broad spectrum cardiovascular benefits without the potential toxicity of statin drugs. Red yeast rice extract outshines statins because it contains an array of naturally-occurring heart-friendly phytochemical compounds (mevinolin, beta sitosterol, stigmasterol, isoflavones, and monounsaturated fatty acids), rather than just one purified drug molecule.
Red yeast rice extract, like statin drugs, reduces levels of coenzyme Q-10, so this must be replaced. Take 50-200 mg a day of Coenzyme QH (the more active, reduced form of coenzyme Q-10).
Drink 6-8 ounces of pure organic pomegranate juice daily.
Pomegranate juice is almost too good to be true. Pomegranate doesn't just lower cholesterol; it also reverses atherosclerosis! And it tastes great too.
Delivering a cornucopia of phytochemical compounds, and rich in polyphenols, pomegranate has been shown to block cholesterol synthesis, melt away advanced atherosclerotic lesions in humans, reduce LDL oxidation, and prevent the accumulation of cholesterol in macrophages that leads to the formation of foam cells. This delicious, sweet ruby red juice also lowers blood pressure by inhibiting angiotensin-converting enzyme (ACE). It reverses the carotid intima-media thickening caused by atherosclerosis. It reduces platelet aggregation, rendering blood less likely to clot, thus reducing risk of thromboembolic disease.
This incredibly versatile fruit serves up potent anti-cancer (breast, prostate, colon, leukemia) and immuno-potentiating effects, and has even been shown to protect against osteoporosis.
If that weren't enough, pomegranate juice is the most powerful fruit-derived antioxidant, and has been shown to reduce oxidative stress everywhere in the body.
Any old pomegranate product won't do. The juice must be pure - no other ingredients, no other juices, and no additives. It must be made from whole fresh fruit, not from concentrate, because processing damages its sensitive phytochemicals. It must be organic. The only brand I have been able to find that fits this description is Lakewood "Pure Pomegranate". Avoid pomegranate in capsules, as processing into a powder denatures some of its more sensitive components.
Why haven't you heard about the wonders of pomegranate juice? Trust me here, if Big Pharma could profit from peddling pomegranate juice, you would have already seen TV ads promoting it as more effective than statins. The drug industry's multi-billion dollar statin market would vanish overnight if the public became aware of the power of pomegranate juice.
Take 2-4 caps twice a day (Inflammation Control; Renewal Research). Make sure the word " Meriva®" appears on the label.
Curcumin (curcumin longa) is the bright orange-colored active ingredient in the popular native Indonesian and South Indian spice, turmeric. Curcumin contains an array of potent antioxidant and anti-inflammatory compounds shown to block many of the molecular biological changes that can lead to stroke and heart attack. Beyond lowering cholesterol and LDL, researchers have shown that curcumin exerts the following amazing array of vascular effects:

Beyond its vascular effects, curcumin displays a remarkable array of healthful, curative, even life-extending properties. Hundreds of research studies have documented curcumin's medicinal effects: anti-cancer, anti-arthritic, anti-inflammatory, anti-depressant, pain-reducing, hepatoprotective, antihypertensive, and antibiotic.
Dose and delivery: 2-8 500 mg capsules twice daily, or use turmeric liberally in cooking. 2-8 grams a day have been used in research studies. Curcumin is not well-absorbed. Purchase only "phytosome" products in which curcumin has been bonded to a fat soluble substrate like phosphatidylcholine to enhance absorption.
Take 1-2 capsules twice daily.
Green tea is the second most consumed beverage in the world (water is in first place). A huge amount of published research - including 25 years of clinical trials in Europe and Asia - has demonstrated that green tea delivers a phytochemical bonanza of health benefits. Rich in flavonoid catechin polyphenol antioxidants such as EGCG (epigallocatechin gallate), green tea not only protects against cardiovascular disease; it also reduces the risk of cancer, impaired immune function, osteoarthritis, infection, gum disease, and even tooth decay.
The LDL receptor (a cell-surface protein that latches onto LDL particles) is the major mechanism by which the liver removes cholesterol from the bloodstream. Low LDL receptor function is seen in individuals with elevated cholesterol. Green tea reduces cholesterol and LDL by increasing LDL receptor expression - i.e., green tea encourages increased production (via gene expression) of LDL receptors (as measured by LDL receptor binding activity, protein and mRNA) - in the liver. By up-regulating the LDL receptor, green tea reduces cholesterol by 30%.
EGCG, the main active component in green tea leaves, protects your cells from oxidative damage by those nasty omnipresent free radicals that can shorten your life by causing cancer, arteriosclerosis, heart disease and accelerated aging. EGCG inhibits oxidation of fats (including the all-important LDL particle), lowers cholesterol, and blocks the development of the clots (called anti-thrombotic activity) that lead to heart attacks and strokes.
The polyphenols in green tea improve blood sugar regulation in persons with insulin resistance.
Green tea protects the endothelium from oxidative and inflammatory damage.
Green tea has been shown to assist in weight loss.
EGCG and other green tea phenols also protect our DNA from ultraviolet and visible radiation-induced damage: at least one researcher has shown that sipping green tea before exposure decreases sunburn.
Black tea leaves contain a little EGCG but much less than the green alternative.
Take 2-4 400 mg capsules twice daily.
Take 4-6 1000 mg capsules daily.
One tablespoon or 6 caps daily. Essential fatty acids lower LDL and cholesterol and provide the raw material for our bodies to synthesize inflammation fighting prostaglandins. Flaxseed oil is as effective as fish oil at reversing heart disease and is preferable for several reasons, not the least of which is that it is not contaminated with mercury.
Take 2-4 1000 mg capsules twice daily.
In 2000 the Mayo Clinic published a review of 18 trials including 823 subjects, establishing that fish oil supplements significantly reduce triglyceride levels. (Motori VM, 2000).
According to American Heart Association's guidelines (AHA Statement 11/18/2002), people who have elevated triglycerides may need 2 to 4 grams of EPA (eicosapentanoic acid) together with DHA (docosahexanoic acid) per day provided as a supplement.
Exercise is essential! One hour every day, divided equally into strength and cardio. All forms of exercise lower cholesterol and LDL. It is unlikely that you can lower your cholesterol and LDL levels without exercise. As an added benefit, exercise has been shown to reverse plaque.
A low thyroid elevates total cholesterol and LDL. Doctors usually miss an elevated cholesterol level when its caused by subclinical hypothyroidism. Undetected hypothyroidism is very common, especially in people over 40. You can't trust your doctor to correctly diagnose hypothyroidism. Anyone with a TSH of 2.0 or more is almost certainly hypothyroid. If your free T3 level is 3.5 or less you are hypothyroid. Take the Basal Metabolic Temperature Test (oral temperature upon arising) on your own at home as described in chapter 36 of my book, Renewal: the Anti-Aging Revolution. (Published by Rodale Press and St. Martin's Press). If your basal temperatures are consistently low (below 97.8), you are definitely hypothyroid. If you have symptoms of hypothyroidism and your TSH is above 2.0 (regardless of what your doctor may tell you), you are hypothyroid.
If you are hypothyroid, you will need to find an alternative/integrative doctor who can prescribe natural Armour Thyroid and do followup testing to make sure you are in thyroid balance.
* I don't recommend taking these. They are included for informational purposes only.
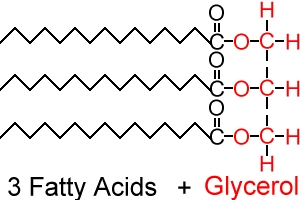
As discussed in the section above on Lipoproteins, the body needs to make fat molecules water-soluble so it can transport them in the blood stream. Triglycerides are the answer. Here's how it works. Start with glycerol, a small molecule that loves to carry fatty acids around. Each glycerol molecule has three attachment sites - three places where it can "hold hands" with a fat molecule. When all three sites are filled, we have a triglyceride.
Glycerol isn't particular about who it holds hands with so long as it looks like a fatty acid: any type of fat molecule can attach to its three sites. They might be the unhealthy, pro-inflammatory saturated fatty acid molecules we find in animal products like dairy, eggs, cheese, poultry, and red meat. They might be the really nasty trans-fats we find in junk, fried, and fast food - or they might be the healthier polyunsaturated oils we find in plant foods and oils. Or the glycerol could be carrying the best fats of all, the essential fatty acids like alpha linoleic acid, which we get from walnuts, olives, and flaxseed oil. Whatever kind of fat they are, they are bound, three at a time, to the glycerol "carrier" as a triglyceride for delivery to their respective job sites.
Triglycerides ride around in the bloodstream alone, but they also get packaged up into larger transport vehicles, the lipoprotein particles discussed earlier in this chapter: HDL, LDL, and VLDL. The triglyceride level that is part of a lipid panel measures only the triglycerides that are free, not those already packaged up inside of LDLs, HDLs and VLDLs.
It should not surprise you that an elevated triglyceride level is very useful for predicting cardiovascular disease risk. Degree of triglyceride elevation predicts both the severity of atherosclerosis and the likelihood of a heart attack or stroke. Multiple studies have shown a near linear relationship between triglyceride concentration and coronary heart disease event rates.
Individuals with high triglycerides are also at high risk of developing insulin resistance (the metabolic syndrome (see Chapter 11).
If your triglycerides are elevated it means there's too much fat in your blood. Obviously, a diet high in fats will raise serum triglycerides. Even though triglycerides are fat molecules, an elevated triglyceride level doesn't necessarily come just from the fats you have eaten; it can also be caused by eating too many carbs.
When we eat too many carbohydrate-containing foods, our body gets rid of the extra carbs - the ones we don't burn off immediately - by packaging them up as triglycerides. So excess carbohydrate consumption causes triglyceride level elevation. Is it no wonder that research clearly shows that reducing carb intake and increasing exercise (to burn off the extra carbs) lowers triglyceride levels and protects against atherosclerosis?
Another separate, but equally serious problem caused by elevated triglycerides is impaired fibrinolysis (clot dissolving). Unless our bodies can get rid of clots rapidly, the likelihood of a stroke or a heart attack increases exponentially.
Finally, triglyceride elevations have the undesirable effect of driving down "good" HDL levels.
So we have many reasons to watch our triglycerides closely and work to keep them in the normal range. (See end of this chapter for treatment recommendations.)
Therapeutic Goal: Lower triglycerides to 150 mg/dL or less.
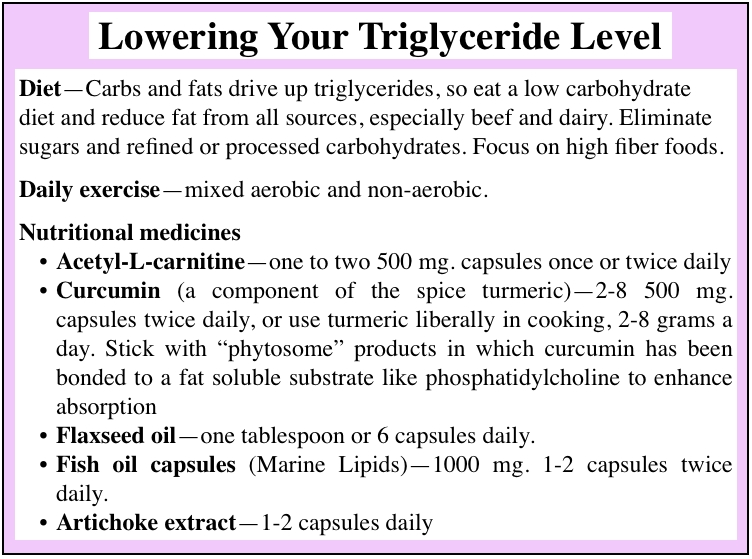
Diet - Carbs and fats drive up triglycerides, so eat a low carbohydrate diet and reduce fat from all sources, especially beef and dairy. Eliminate sugars and refined or processed carbohydrates. Focus on high fiber foods.
Daily exercise - mixed aerobic and non-aerobic.
Eat more fruits, vegetables, and beans.
A low-carbohydrate diet is essential for lowering triglycerides because excess carbohydrates drive triglyceride levels up. Eliminate all refined carbs and sugars. Small quantities of unprocessed, complex carbohydrates (beans, nuts, seeds, whole grains) are acceptable. Eliminate sweets and all foods that contain added sugar, including juices, baked goods, processed foods, and snacks.
Low-fat diet. All dietary fats, but especially animal fats and hydrogenated oils, elevate triglyceride levels.
Acetyl-L-Carnitine (ALC) (500-1000 mg once or twice a day). Acetyl-L-Carnitine's primary role in the body is to transport fats (triglycerides) into our mitochondrial energy factories so they can be used as fuel. ALC accelerates the burning of fats by shuttling them into your heart muscle cells to be burned for energy. Without ALC, fatty acids (TGs) are unable to penetrate the membrane of the mitochondria, resulting in a decreased rate of fat utilization and energy, and a weaker heart muscle. ALC is not an amino acid; it is a vitamin-like nutrient related to the vitamin-B family. When subjects with hypertriglyceridemia (elevated triglycerides) were given 900 mg per day of supplemental ALC, blood triglycerides plummeted from an initial value of 440 mg/dL to 186 mg/dL after eight weeks of treatment. ALC also lowers cholesterol and improves cognitive functioning.
Flaxseed oil (1 tablespoon or 6 capsules daily).
Marine lipids (3-5 1000 mg capsules daily). In hundreds of studies DHA and EPA in this dose range have consistently shown triglyceride-lowering properties. A 2000 Mayo Clinic review of 18 trials including 823 subjects established that fish oils significantly reduced triglyceride levels. In 2002 the American Heart Association's guidelines for people with elevated triglycerides included a recommendation to take 2-4 grams daily of the two main components of marine lipids: EPA (eicosapentanoic acid) and DHA (docosahexanoic acid).
Garlic and onions or garlic extract capsules (2-4 twice a day).
Curcumin - 1-8 grams a day of turmeric or 4-8 capsules a day of Inflammation Control (Renewal Research). See description of curcumin in "Basic program to lower Cholesterol and LDL" above.
Multivitamin - Renewal Research (or another top quality multi) daily; take amount recommended on label.
Cinnamon extract (Cinnulin®) - A study reported in Diabetes Care showed that after 40 days of treatment with Cinnulin® cinnamon extract, triglyceride levels in 60 patients had dropped 23-30% as compared with controls given a placebo.
Artichoke extract - Several studies have shown that artichoke blocks cholesterol production in the liver and lowers triglyceride levels.
Chromium (200-1000 mcg daily).
Exercise is very important! One hour daily, cardio and strength. All forms of exercise lower triglyceride levels. Get used to this idea: the triglyceride research literature strongly suggests that it is unlikely you'll be able to lower your triglyceride level without daily exercise.
Modest Weight loss (10-15 lbs.) can greatly reduce your triglycerides.
Make sure you are not hypothyroid. Undetected hypothyroidism is very common and causes triglycerides to go up. Take the Basal Metabolic Temperature Test on your own at home as described in chapter 36 of my book, Renewal: the Anti-Aging Revolution (published by Rodale Press and St. Martin's Press). If your basal temperatures are low (below 97.8), you are hypothyroid. If you have symptoms of hypothyroidism and your TSH is above 2.0 (regardless of what your doctor may tell you), you are hypothyroid. If your free T3 level is below 3.5 pg/ml, you are hypothyroid.
* I don't recommend taking these. They are included for informational purposes only.
High-density lipoproteins (HDLs), the smallest lipoprotein particles, are about one-third the size of LDLs and carry about one-third of all the blood cholesterol. In the submicroscopic nanoscale world of lipoprotein particles, HDL is the veritable "good guy," the hero who specializes in protecting us from the nasty LDLs that cause atherosclerotic plaque.
Like LDL, HDL is made in the liver, and plays a very important role in cholesterol metabolism: HDL finds and latches onto cholesterol molecules, and then escorts them back to the liver so they can be booted out of the body. We call this "reverse cholesterol transport".
HDL is kind of like the sheriff: its sole mission is to ride out and nab excess cholesterol molecules, handcuff them, and then deliver them to the liver, which then expels them from the body. By taking up the extra cholesterol, HDL prevents LDL from grabbing it. That's one reason (of several) why HDL is famous for reducing the risk of atherosclerosis. Though HDLs are known as "good cholesterol," the cholesterol molecules they carry are identical to the cholesterol in LDL (so-called "bad cholesterol") particles. HDL's ability to remove extra cholesterol and dispose of it is what makes it "good".
HDL particles go beyond merely removing excess cholesterol from the bloodstream; they also possess the unique capacity to remove cholesterol that has already been deposited in atherosclerotic plaque.
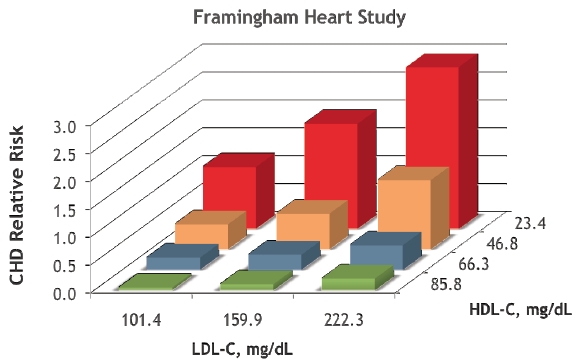
Because HDL particles offer powerful protection from heart and vascular disease, you want more of them. You don't need many more, however, because small changes in HDL translate into big changes in risk: each increase of 1.0 in the HDL number (measured in mg/dL), corresponds to a 3-4% reduction in coronary heart disease risk. So, for example, a five point increase lowers risk by up to 20%.
Low HDL levels are commonly found in people who are sedentary, smoke, are overweight, have insulin resistance (see Chapter 11), have elevated triglycerides, or have chronic inflammatory disorders (see Chapters 10 on fibrinogen and 8 on C-reactive protein).
Individuals with higher HDL levels ( > 40) have much lower rates of cardiovascular disease, while those with low HDL ( ≤ 40) have increased rates.
Low HDL cholesterol is a major, common, independent risk factor for coronary heart disease (CHD) and ischemic stroke, and this risk is present even when total cholesterol levels are normal.
Low HDL cholesterol is often associated with high triglyceride levels. Anything that causes high triglycerides will usually also lower HDL, and conversely, if triglyceride levels are high, lowering them raises HDL.
The most recent report of the National Cholesterol Education Program identified low HDL cholesterol as an independent coronary artery disease risk factor and recommended that "all healthy adults be screened for both total cholesterol and HDL cholesterol levels".
Recent landmark clinical studies have demonstrated diminished mortality and first coronary events following elevation of (a previously) low HDL cholesterol level. The Framingham Heart Study (a famous long-term atherosclerosis research study) produced compelling evidence that a low level of HDL cholesterol was an independent "predictor" of coronary artery disease.
For all of the markers I discuss in this book except HDL, lower levels are better. HDL is the one exception: more is better. An ideal HDL level is at least 40, preferably in the 50s, and the lowest possible risk is at 60 or more. If your HDL is low (i.e., below 40), use the information at the end of this chapter to design and implement a personal program that will raise it up to healthy levels.
When oxidized LDL particles find their way into your arterial wall (see chapter 5 on Atherogenesis), monocytes (small white blood cells) follow them in. Once inside the arterial wall, these monocytes morph into much larger cells called macrophages, which then proceed to gobble up (we call this phagocytosis) LDL particles and the cholesterol they contain. These fat-engorged macrophages grow to an enormous size, too big to get back out of the arterial wall, so they become trapped there and die. The buildup of cholesterol and debris from dead macrophages causes plaque.
HDL particles abort the above-described process, thus thwarting atherosclerotic plaque formation. HDL literally snatches extra cholesterol molecules away from the jaws of the macrophages about to devour them. Then HDL then gently ushers the cholesterol back into the bloodstream, and then to your liver, which expels it from your body.
Beyond retrieving cholesterol from atherosclerotic plaque deposits and taking it back to the liver, HDL particles demonstrate other properties that may contribute to its ability to protect us from atherosclerosis. HDL particles carry many lipid and protein species, several of which are biologically very active despite very low concentrations. These compounds exert influences that block and reverse atherosclerosis: they inhibit oxidation, decrease inflammation, activate the endothelium, reduce platelet activation, and control coagulation.
Raise HDL to at least 40. Ideal level is 50 or more.
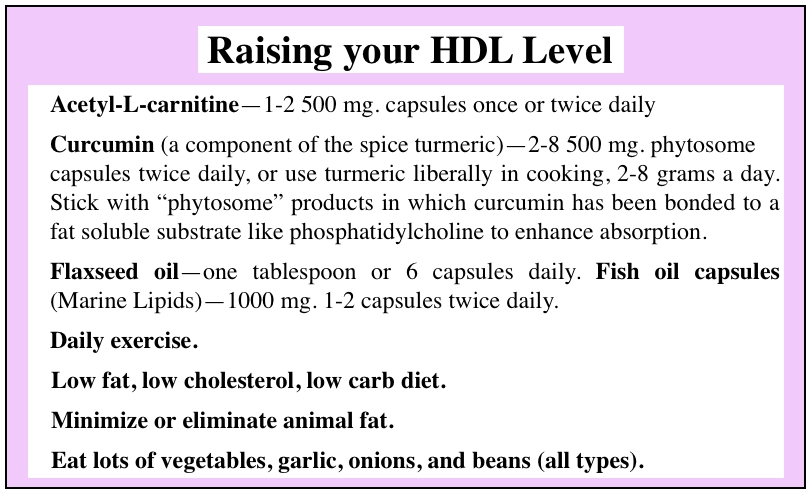
Acetyl-L-carnitine - 1-2 500 mg. capsules once or twice daily
Curcumin (a component of the spice turmeric) - 2-8 500 mg. phytosome capsules twice daily, or use turmeric liberally in cooking, 2-8 grams a day. Stick with "phytosome" products in which curcumin has been bonded to a fat soluble substrate like phosphatidylcholine to enhance absorption.
Flaxseed oil - one tablespoon or 6 capsules daily.
Fish oil capsules (Marine Lipids) - 1000 mg. 1-2 capsules twice daily.
Low fat, low cholesterol, low carb diet.
Minimize or eliminate animal fat.
Eat lots of vegetables, garlic, onions, and beans (all types).
Aerobic Exercise. This can be done in many ways. Examples are jogging or fast walking one hour a day. Your heart rate will tell you whether you are in the aerobic range or not.
Low cholesterol diet. Animal foods (all meat and dairy, eggs) contain cholesterol; plant-derived foods do not.
Curcumin is a component of the Indian spice turmeric. (E.g. Inflammation Control, Renewal Research, 2-4 capsules twice a day.)
Acetyl-L-Carnitine (ALC) - By facilitating the intracellular cellular processing of fats, ALC pushes HDL upward. (500-2000 mg a day) Also supports brain health and cognitive function.
A top quality daily multivitamin-mineral.
Fish oil capsules (1000-4000 mg a day; Marine Lipids, Renewal Research).
Flaxseed oil (one tablespoon or 6 capsules daily).
Garlic, either dietary or as a daily supplement (2-4 capsules twice a day).
* I don't recommend taking these; they are included for informational purposes only.
Very Low Density Lipoprotein (VLDL) is type of lipoprotein particle that is structurally identical to LDL, but much bulkier. Assembled in the liver from cholesterol, triglycerides, and special proteins, the largest VLDL particles have a diameter of 30-80 nm.
Because of their size, VLDL particles contain a particularly high proportion of lipid in the form of triglyceride molecules. As VLDLs circulate through the bloodstream, their size decreases as they gradually release triglyceride molecules (which are burned off by fat and muscle tissue). Thus they gradually shrink to become low density lipoprotein (LDL) particles.
Too many VLDLs are worrisome for all the same reasons we worry about excess LDL. Elevated VLDL levels accelerate atherosclerosis and an elevation is closely associated with vascular disease in the heart, brain, and elsewhere.
VLDL may also be elevated in other diseases and metabolic states that involve inappropriate processing of lipids. The one most important to readers of this book is the metabolic syndrome, which is the subject of Chapter 10.
Lower your VLDL to below 40 mg/dL.
VlDL levels go up and down in tandem with LDL and cholesterol. Therefore, the methods listed above for lowering cholesterol and LDL will be equally effective at lowering your elevated VLDL.