Superior Index Go to the next: Chapter 6
Print Files: A4 Size.
My patient, Robert Barnes, is a charming, engaging, and delightfully inquisitive university physics professor. Convinced that knowledge is power, Bob insists that I tell him exactly why his coronary arteries have hardened to the point where he's had a heart attack ...
"Doc, I exercise every day, I eat right, and I feel great. My cholesterol is under control. I don't have hypertension. I don't smoke. Every year my internist has been telling me my lipids are great and I have nothing to worry about. So why would I have a heart attack? I know I didn't just wake up last week with heart disease. This must have been developing gradually, right?"
"That's correct, Bob. Even though you had no warning in terms of symptoms, your myocardial infarction didn't happen overnight. The atherosclerotic hardening and plaque formation in your coronary arteries has been progressing gradually and silently for perhaps twenty or thirty years. Until two weeks ago - which was when you felt the chest pain, shortness of breath, and sudden weakness - you weren't aware of anything going on in your heart. The Emergency Room doctor explained that you had suffered a mild coronary - a heart attack. You were admitted for observation overnight, and discharged the next day. Even though the first symptoms were cataclysmic, the process that led up to it had been developing for decades."
"Yes, several decades. For many victims, coronary hardening and plaque formation begins in childhood. It doesn't surprise me that your doctor didn't know about it. Most doctors don't order the necessary tests, even though it's easy. Nowadays we can identify this killer disease process at the earliest stages and reverse the factors that cause atherosclerosis long before problems arise."
"Yes, we can. Welcome to modern molecular medicine, Bob."
"Then tell me why. Why was that happening? What exactly is atherosclerosis, anyway?"
"If you have a few minutes, I'll explain the entire process."
"This is unbelievable! A doctor who explains things to his patients. How refreshing!"
"I have found that patients who understand the origins of their disease are far more likely to succeed at reversing it. Heart patients often go to their doctor hoping to get a magic pill that will somehow make the problem disappear. Physicians encourage this delusion by whipping out their prescription pads, which sends a powerful unspoken message that taking a drug or having surgery will somehow make the problem go away. Though the drugs may help control the symptoms, the underlying problem will not go away unless we identify and remove its causes. So you really need to know how you got into this pickle."
"It's important to appreciate how an artery is constructed, so I am going to start with a brief anatomy lesson. Then I'll explain atherogenesis - that's the technical term for the development of atherosclerotic plaque. It's a little complicated, but you'll be able to follow. Once you have your arterial anatomy down and understand how plaque develops, then I am going to explain how an actual heart attack happens. Later on, you'll learn how to use biochemical testing to `see' atherosclerosis long before it becomes a problem. Then I'll show you how to use natural medicines to reverse it."
"Doc, you have an organized mind. I like that. Okay, first the anatomy lesson."
"Your heart is an amazing organ. It beats more than 100,000 times a day and about two billion times in a life. Your heart pumps five quarts a minute or 2000 gallons a day. Your cardiovascular system - including arteries, capillaries and veins - is over 60,000 miles long, more than twice the distance around the earth."
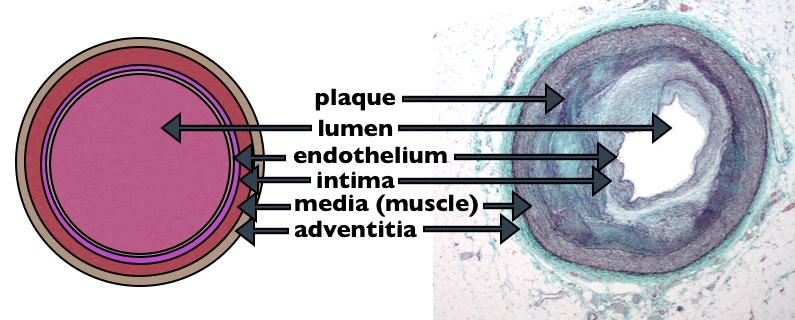
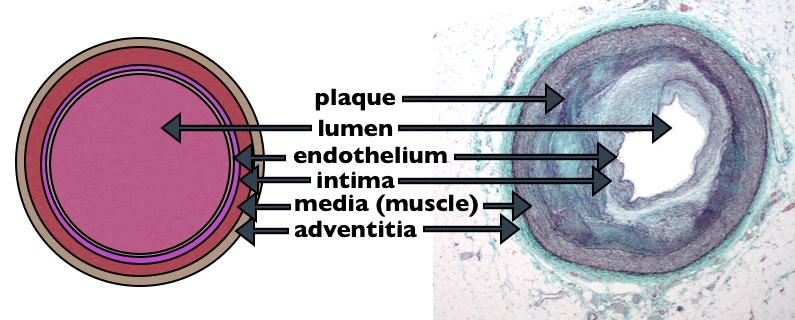
"An artery is a lot like a very small hose. This particular hose has four layers. Starting from the inside (we call it the `lumen') and working toward the outside, we'd first encounter a very thin, single layer of cells, called the endothelium. Endo means `inner,' and `thelium' means `skin'. As you will see, the endothelium is the most important part of any artery. This is because of its very special position as an interface - a barrier - that separates the blood flowing through the artery from the wall of the artery. The endothelium is a very selective membrane that allows nutrients and other desirable substances access to the inner layers of the artery while keeping toxins and other undesirables out."
"Beneath the endothelium (working now from the center, or lumen, outward) is a much thicker elastic band of connective tissue called the intima. The intima gives the artery elasticity and flexibility. Beneath the intima (still working from interior to exterior) is the media, a thick layer of muscle cells that contracts to change the size of the artery. And finally, on the outside is the adventitia, an outer protective band of tough elastic fibers that provides structural strength and holds the whole thing together."
"Atherosclerosis, Bob, is the body's response to vascular injury - or damage to an artery. I am going to show you how this injury happens."
"There are four major phases in the development of atherosclerosis and the heart attack and stroke it causes. The first phase is endothelial damage and dysfunction. The second is plaque formation, and the third is thrombus formation."
"The endothelium," I continue, "that paper-thin inner lining of your arteries holds the key to understanding heart attacks and coronary artery disease. Atherosclerosis - and all the human misery it causes - begins there. The endothelium's power is all out of proportion to its size. Just one cell thick, it comprises a very small percentage of the total size of an artery. But, as any real estate agent can tell you, location is everything. Because of its strategic location guarding the interface between blood and artery, the endothelium wields tremendous influence."
"As gatekeeper to the arterial wall, it functions as both a protective barrier and selective membrane. It sorts through all the good and bad chemicals floating in the bloodstream (nutrients, hormones, electrolytes, proteins, cell-signaling molecules, waste material, metabolites, etc.), and decides which to allow through to the arterial wall below. Your endothelium is also a chemical factory: it manufactures special molecules that keep it healthy. And, if it senses damage, it will produce chemical messengers that call in the immune police force.
"Atherosclerosis, The `Number One Killer,' begins when the endothelium is irritated or damaged. This causes it to malfunction, and it can no longer effectively protect the rest of the arterial wall. Oxidized LDL-cholesterol particles flowing through the bloodstream can now penetrate below the injured endothelium and embed themselves in the wall of the artery. Plaque is born."
"So that's why there's so much emphasis on cholesterol?"
"Yes. Cholesterol is important because if the endothelium is compromised, cholesterol (actually just oxidized LDL particles) will gain entry into the artery, and this initiates and/or accelerates the atherosclerotic process."
"Now let's imagine we can shrink ourselves down and travel together to the center of one of your coronary arteries, in order to see what happened to the endothelium there."
"Unlike the arterial cells beneath it, the endothelium is exposed to everything that flows through the bloodstream, and that bloodstream can carry some very nasty molecular entities. These bang into the endothelium, irritate it, and cause it to become inflamed."
"Not a good thing?" he offered, tongue in cheek.
"No, Bob, it's not. Since this is the initial event that leads to atherosclerosis, the disease that kills most of us, I'd say it's a very bad thing."
"Endothelial irritation is the initial step in a chain reaction that progresses to inflammation, then damage, then dysfunction, atherosclerosis, and finally culminates in a heart attack or stroke."
I opened a book and showed Bob the following list:
"That's a long list! Tell me, doc, how can I start protecting my endothelium from damage?"
"Exercise every day, for an hour if possible. I can't emphasize this strongly enough. Keeping your blood vessels strong and healthy through exercise is arguably the most important single thing you can do to protect your endothelium from damage."
"Eat a low-carbohydrate diet: too much sugar and processed carbohydrates are very damaging. Eat organic whenever possible. Keep animal fat at a minimum, because it increases free radical burden. Instead, use moderate amounts of vegetable fat (like coconut, olive, flaxseed, and soy bean oils) along with small servings of very lean meat. Load up on phytonutrient-rich fruit and vegetables. (For a thorough discussion of phytonutrients, see chapter 25 in my book, Renewal: The Anti-Aging Revolution.)"
"Every day, make sure you take plenty of nutritional supplements: a multivitamin, extra vitamins C and E, flaxseed oil, and coenzyme Q-10. Antioxidant-rich phytochemical foods and supplements such as pomegranate, blueberries, grapeseed extract, green tea, pycnogenol, milk thistle, and bioflavonoids."
"Some common dietary sources of endothelial irritants include: a high-animal-fat diet, trans-fats, processed foods, chlorinated water, and pesticides."
"Virtually all chemical toxins irritate and injure the endothelium. Pesticides, herbicides, air and water pollutants, heavy metals (lead, arsenic, mercury, cadmium), tobacco smoke, sugar, and alcohol. Free radicals damage the endothelium. (For a more complete discussion of toxins and free radicals - where they come from and how to manage them - see chapters 2 and 11 in Renewal.)"
"Measure and treat (if they're elevated) the three markers for arterial inflammation: homocysteine, C-reactive protein, and fibrinogen. I'll have a lot more to say about these rascals later on. For now, I want you to remember that these undesirable irritants cause endothelial damage, and that lowering your body's level of them will prevent, reverse, and even cure hardening of the arteries." (See Part II of this book for details about these markers.)"
"Blood sugar problems also cause endothelial inflammation. Syndrome X, insulin resistance, excessive insulin, and elevated fasting blood glucose fall into this category. Persistently high blood sugar levels (greater than 90 mg/dL) result in endothelial damage that accelerates atherosclerosis. (For more on this subject see Chapter 11 - Blood Sugar, Insulin Resistance, and The Metabolic Syndrome.)"
"As a physicist, Bob, you might appreciate that mechanical stress can also trigger endothelial damage. High blood pressure causes excessive `shear stress.' In hypertension, the heart has to beat harder, and this increases the pressure on the endothelial surface and raises the friction caused by blood passing along the endothelium. Because these effects of hypertension are so damaging, it is very important to make sure your blood pressure is normal."
"Several infectious agents are known to damage the endothelium and cause coronary artery disease. These include periodontal (gum) infections, herpes virus, Chlamydia, cytomegalovirus, Helicobacter pylori, and Candida (yeast)."
"Allergies and autoimmune diseases (where the immune system makes antibodies that attack one's own tissues) also stir up inflammation that damages the endothelium. Untreated hay fever (allergic rhinitis), sinusitis, asthma, food allergies, rheumatoid arthritis, lupus, multiple sclerosis, and Hashimoto's disease can increase your risk of heart attack."
"Okay, I think I get it now, doc," says Bob. "Virtually anything that can cause inflammation will damage the endothelium, right?"
"Right. But endothelial inflammation - from some combination of all the causes I just listed - is just the beginning."
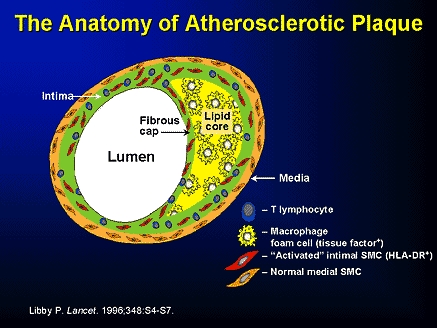
"Healthy endothelial cells protect the intima , the layer of arterial wall that lies beneath. When the fires of inflammation have damaged endothelial integrity, however, LDL particles now can gain access to the intima."
"Aha!" says Bob. "So the LDLs get into this place where they don't belong. That's why they cause such big problems. I've always wondered about that."
"You're right, but it's a bit more complicated. As they become trapped between the endothelium and the intima, LDLs are oxidized by the free radicals that were generated by the local inflammatory reaction. In response to the oxidized LDL, the inflamed endothelium senses danger, goes into `alarm mode'."
"Endothelial cells manufacture and release messenger molecules that tell the immune system to send in its monocyte cells. Monocytes, a kind of white blood cell, are the cellular police force."
"Several ways. They are mobile, attracted to problem areas, carry weapons - and they have an `attitude.' Their job is to take over and control situations they deem `dangerous' (real or perceived). Monocytes can use their communication system to call in reserves if needed. An inflamed blood vessel wall like the one I've been describing, coupled with some oxidized LDL, is definitely perceived as a dangerous situation."
"Under normal conditions," I continued, "monocytes in the bloodstream, like police on patrol, would have just slid on by, but now they migrate toward and adhere to this sticky inflamed endothelial surface. Then, on the trail of the oxidized LDL, they, too, go through and below the endothelial cell and embed themselves in the intima."
"In pursuit of perps?" offers Bob.
"Yes, but now things get weird. Once safely beneath the surface layer of endothelial cells, these monocytes do something real cops could never do: they rapidly increase their size by several times, transforming into another type of white blood cell, the macrophage."
"Okay, I'll bite - what's a macrophage?"
"Macrophages are a kind of huge immune system supercop cell. Their enormous size allows them to more easily engulf things, and when they are munching on toxins and viruses, on fungal cells and cancer cells, we are very happy with their behavior. But just like good cops gone bad, when they get into the inside of your blood vessels and start gobbling up cholesterol and oxidized LDL ... well, we have a friendly fire situation. They do more harm than good.
"They actually eat the oxidized LDL?" asks Bob.
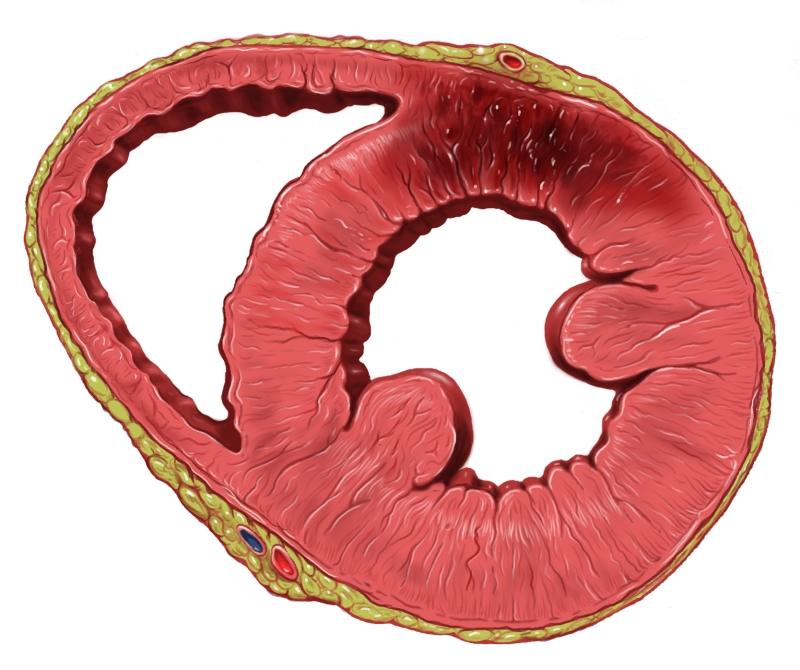
"Yes. We call it `phagocytosis.' Here's how it works: a macrophage snuggles up to one of the LDLs, and then sends out two `arms' of protoplasm that surround it in a deadly hug, and then close in from behind, totally engulfing it, so that now the LDL is actually completely inside of the macrophage. Instead of simply gobbling up a few of the oxidized LDLs and digesting them, however, these macrophages overindulge; they can't stop eating, so they become engorged with fat. The fat that they have been eating, however, is lethal to them. They die, but not before they grow so large that they can't get back out of the arterial wall, so they become entombed there. The LDL-engorged carcasses of these dead macrophage supercops accumulate in the intima, and consolidate to form plaque. On a microscopic slide preparation these dead cells take on a bubbly appearance, and have come to be called `foam cells.' When sufficiently large numbers of foam cells accumulate, fatty yellow streaks appear. These protrude above the interior surface of the artery into its lumen; this narrows the vessel and reduces its capacity to carry blood. We call this ischemia. Ischemia in brain blood vessels causes cognitive problems. Ischemia in heart vessels causes chest pain, fatigue, and shortness of breath. And, of course with atherosclerotic blockage you have increased risk of heart attacks and strokes."
"So that's the end of the second phase, which you called plaque formation?"
"Right, Bob. The third and final phase is thrombus formation."
"I guess it really is `final' for some people."
"Bad joke, Bob. But sadly, it's true. You've probably also heard this one: `The first symptom of a heart attack is often sudden death.' This is the unfortunate truth for about half of all heart attack victims."
"Now that you have my attention, exactly what is a `thrombus,' doc?"
"It is simply a blood clot - a very dangerous kind of clot that occurs inside an artery. But we are getting ahead of ourselves. First you need to know about unstable plaque. On the way to eventually becoming `stable plaque,' these fatty atherosclerotic deposits go through a dangerous phase known as `unstable plaque,' in which a very thin layer of connective tissue cells forms a thin, fibrous cap that covers over the fatty plaque lesions I've been describing. It's a lot like the thin scab that you can see soon after an external cut or scrape on your skin. This cap sits on top of the foam cells in the fatty streak, forming a `bump' that protrudes even further into the lumen (the inside) of the vessel."
"Calcium," I continued, "is now attracted to the area and deposits there, causing the plaque to harden, or `calcify.' This causes the plaque to gradually become less elastic and more brittle, like thin bone, and it can now easily break."
"This combination of foam cells, calcification, and lipids, covered over by a fibrous cap, is what we call `unstable plaque.' It's kind of like a festering sore, or boil, and it's especially dangerous, because, as you can see, the normally soft and pliant connective tissue `cap' that covers it has now become hard, fragile, and brittle."
"Beneath this fibrous cap," I continued, "trapped foam cells are dying and in their death throes they release harmful chemicals that push upward, encouraging the fibrous cap to rupture. If the cap does rupture, all heck breaks loose. It's like a pimple or boil erupting: toxic contents are spewed out. A clot, or thrombus, starts forming right there on the inside wall of the artery. If this clot becomes large enough, it will cause local blockage of downstream blood flow (called an `infarction') in the affected artery. Or the developing clot can break loose and travel downstream, quickly lodging in a narrower portion of the artery. Either way, this is what we call a cardiovascular `event.' If this `event' occurs in the heart, it's a myocardial infarction. The victim suffers sudden chest pain, fainting - and as often as not, death. If the blockage happens in the brain, we call it a stroke, or cerebral infarction and the patient suffers loss of cerebral function or death."
"This complex atherosclerotic process I've just described usually remains silent - in other words, there are no symptoms. And without symptoms, there's no way to know it is developing. No medical procedure or imaging technique can detect an unstable plaque on the verge of rupture. Nothing like a heart attack attention."
"I can vouch for that! But now we have a way to know that train wreck is coming. Now we can do the six tests you recommend."
"And then we can use your molecular medicine program to reverse the causes of heart attacks before they happen?"
"You are a perceptive fellow, I must say! Now, thanks to these new discoveries, long before disaster strikes we can use our knowledge of cellular and molecular biology to prevent this disease. If we do our molecular homework, there'll be no reason for plaque to form and rupture, causing these cataclysmic, life-changing - and often life-ending - events. Get tested! Find those biochemical signs of plaque development! Nip this disease in the bud."
"That's why I'm here, Dr. Tim. To learn how to do that. Thanks for the explanation."