Superior Index Go to the next: Chapter 2
Print Files: A4 Size.
It was 2:45 AM. I was sixteen years old and asleep in my bed. In the distance someone moaned "I can't breathe!" Just a bad dream, I thought, and drifted back to sleep. But there it was again ...
Suddenly wide awake, I recognized my father's voice coming from down the hall. There was a kind of urgency in it that I'd never heard before.
I jumped up and dashed to my parents' bedroom. Dad sat on the edge of the bed, slumped forward, breathing hard, clutching his chest - his face pale, almost bluish. Mom was biting her lower lip the way she always did when she was real worried.
"It feels like there's an elephant standing on my chest," Dad groaned.
"What do you think it is, Harry?" asked Mom.
"I don't know. Maybe a little indigestion - something I ate for dinner," replied my father. "Just `a piece of underdone potato' ... "
My father's endearing way of dealing with scary stuff was to make light of it, and there he was, at it again, trying to calm us with a joke/quote from Dickens' A Christmas Carol. Cute - but I wasn't buying it. I figured my parents might fritter away valuable time debating the possibilities, so I picked up the phone and dialed our family physician, Dr. Hess, who - amazingly - answered on the second ring. He asked a few quick questions, then told me, "Tim, your dad's having a heart attack. You need to get him to the hospital right away. Do you have a car?"
"Get him over to the ER as fast as you can. I'll meet you there."
"Oh, okay. Thanks," I stammered. "Sorry to bother you in the middle of the night ... " As I struggled to express my appreciation he interrupted me with five words that changed my life. "That's what your doctor's for. Now get your dad to the ER."
We jumped in the car and fifteen minutes later an EKG at the hospital showed Dad was indeed suffering a myocardial infarction.
In the middle of an emergency, you don't have time to think about what you do and why you do it - you just do what needs to be done. Later on, though, I had a couple of realizations. The first was that Dr. Hess - with those unforgettable words - had shown me that he cared, that he had a heart. "That's what your doctor's for." Wow! This guy, rousted from sleep, had every reason to be grumpy, but instead he sincerely viewed the situation as an opportunity to help. I remember thinking that if I ever became a doctor, that was the kind of doctor I wanted to be. When I'm called in the middle of the night, or a particularly demanding patient is hassling me, or when my work load seems overwhelming and I just want to get away, Dr. Hess' words - and even the sound of his voice - pop back into my head, reminding me how important it is for a doctor to care.
The spirit of "That's what your doctor's for" extends to this book. I have been blessed with a multifaceted career that has guided me toward a unique understanding of how to prevent and reverse our "Number One Killer," atherosclerotic heart and cardiovascular disease - and if that information someday saves your life or that of a loved one, perhaps I will have lived up to the standard set by Dr. Hess on that frightening night half a century ago.
Another realization came years later. When Dad was in the midst of his heart attack, it never occurred to me that he might actually die. His chances of croaking on the spot, were, in fact, about fifty-fifty - and if he had, my life would have been so very different in so many ways that it's frightening to think about it. My father was such a strong, supportive figure that without him I would not have had the moral (not to mention the financial) support I needed to complete medical school. If Dad's heart attack had killed him, I wouldn't be sitting here writing a book about how to prevent death from a heart attack.
Here's another irony: In the fifty years since that night, atherosclerotic plaque - I'm tempted to call it atherosclerotic plague - remains just as deadly as it was then. This is true despite the awesome achievements of modern medicine. Research into cell and molecular biology has shown us the exact mechanisms by which atherosclerosis kills. We have also learned about natural medicines that address - and reverse - the specific biochemical causes of the disease. Unfortunately, this valuable information is not yet applied in clinical practice. We're still chugging along in the Model T of drugs and surgery while a molecular biological Maserati gathers dust in the garage.
My senior year in medical school was capped of with a required six-month rotation in surgery. For one of those months, my classmates and I "shadowed" a surgeon. Each of us was assigned to a different university staff surgeon whom we followed religiously, day and night. If our surgeon was called in the middle of the night, we got up too. If our surgeon was summoned to the ER, we went too. This exercise in immersion allowed us to see and do everything typically done in a busy surgical practice.
It was my great good fortune to have been assigned to cardiovascular surgeon par excellence Humphrey Swank, M.D., generally acknowledged as the local hotshot. Revered by all - especially us wannabe docs - Swank had been immediate past president of the county medical society, and had won numerous other awards and accolades. His reputation as a surgeon's surgeon was deserved. The chance to study with him represented a great learning opportunity and my classmates were green with envy. ("You got assigned to Swank? Whoa!")
Looking back from a more mature perspective, I wonder now why anybody would relish the opportunity to get up at 4:30 AM for rounds, scrub in for surgery at 6:00, then stand in one place for many long hours viewing one grisly surgical scene after another - witnessing some patients come back to life and others die. But I did relish it. At the time the blur of pacemaker insertions, cardiopulmonary bypasses, carotid endarterectomies, valve repairs and replacements, and aortic aneurysm repairs all seemed pretty exciting.
I'll never forget my first day with Swank. He had a gentlemanly warmhearted air about him that helped me realize immediately why everyone - profs, hospital staff, patients, and students - loved him. He welcomed me with a strong handshake and a big friendly smile. His first words to me were, "I trust your experience with me this month will be gratifying." The way he said it suggested more expectation than hope, as if it were my job to make sure my experience was rewarding. "You're going to see a lot of interesting stuff in the next month," he continued. "You'll be scrubbing in with me for every surgery. We'll see all the in-hospital patients on rounds together and you'll sit with me in my office for all the outpatient appointments. Can you hold retractors? Suture? Stand in one place for eight hours without a break if necessary? Endure repetitive questions from anxious patients?"
"Yes, sir". I answered, with all the exuberance of a medical student in the presence of a surgical god.
"Well, then, Dr. Smith, let's scrub in."
Surgeons tend toward brashness - sometimes to a fault - but Swank never slid across that thin line that separates self-confidence from arrogance.
Later that morning, having completed a couple of pacemaker insertions and a valve repair, on our way to a late lunch, Swank told me, "Tim, I've been at this for 35 years now, and the heart continues to amaze me. Other organs multitask but the heart serves just one purpose: that of pushing blood through the body. It contracts and relaxes about 100,000 times every day. You have already studied the precise pathways blood follows as it flows through the various chambers and vessels. In your lifetime, your heart will pump about a million barrels of blood. If blood were oil, that would be enough to fill three supertankers."
Between morning surgery and afternoon rounds, Dr. Swank insisted on hosting me for lunch at the exclusive City Club. Hoping I'd choose a career in surgery and maybe even follow in his prestigious footsteps, he wanted to familiarize me with the some of the extra perks of the hot shot surgeon experience. Every weekday for my month with Swank, we had a fabulous lunch (especially when compared with the humble soup or sandwich my frugal student's budget would have otherwise allowed). I sipped away at my Calistoga water while he knocked back a couple of martinis and told wonderful tales, all true - ranging from his surgical feats to unvarnished tidbits about his personal life - which was clearly in shambles. A nasty divorce. Greedy lawyers. A disappointing teenage son. The thrill was gone ... except for the surgery. I started wondering whether the stress of his life made it all that special. Then, entering another world, we'd hop back into his snazzy red 1969 Oldsmobile Toronado convertible, cruise back to the medical school, and zip through rounds - popping in on the same patients we'd had our hands inside of that morning, or a day or two before. We'd visit three or four different local hospitals and see a couple dozen cases before calling it quits. Two days each week we'd do initial interviews and outpatient follow-up in his splendid 15th floor office, featuring an entire wall packed with degrees, diplomas, and honors showcasing his accomplishments.
My month with Swank had been exciting and intellectually stimulating, but as it drew to a close, something gnawed at me. It wasn't the gory scenes; in medicine one gets used to blood and guts. It wasn't the hideous hours; getting up early and working long hours was standard fare. Nor was it the guy's personal problems; all too often that comes with the territory. Finally I figured it out: woven into the fabric of Dr. Swank's wonderful work - all those high-tech repair jobs - was a backdrop of futility. Specifically, it occurred to me, nobody was getting cured. Sure, Swank provided some extra mileage for worn out hearts, but none of his skills addressed the underlying atherosclerotic disease process that had caused his patients' problems in the first place. I wanted - I needed - to figure out how to close the barn door before the horses had bolted. I figured there must be a way to prevent these heart attacks and strokes. At the time I had no way of knowing it would take a few decades - and over 40 million more deaths - before molecular biology would finally solve the riddle of atherosclerosis.
My first clue about the overwhelming seriousness of the atherosclerosis problem came in my third year of medical school.
Any doctor can tell you that physicians-in-training - and their professors - exhibit a strong tendency to get excited about the "zebras" - the rare, unusual, and thought-provoking diseases - while ignoring the boring everyday "chickens". Backaches, PMS, and the common cold are chickens. Thrombotic thrombocytopenic purpura and Charcot-Marie-Tooth disease are zebras. While we may have learned more by focusing on the zebras, we really needed to learn about the chickens too, because those would be the ones we would see and treat most often. Atherosclerosis turns out to be one humongous chicken.
My freshman and sophomore years in medical school had been all about the necessary but borrrrring basic sciences: anatomy, physiology, biochemistry, pathology, pharmacology, microbiology, etc. When we weren't studying books, we spent our time sitting in lecture halls, peering intently into our microscopes at microbes and tissue samples, or dissecting our cadaver. The only contact with real, live patients was when an occasional "case" was wheeled into the lecture hall or surgical amphitheater and presented to all 100 of us simultaneously. Junior year the fun began. We got to dress up in whites and hit the wards and clinics, acting like real doctors, interviewing and examining real live patients with real diseases rather than the ones we studied on pathology slides and pickled organs. We were pumped about that.
The first week of junior year found me in a hospital ward conference room with about fifteen classmates, bantering as we waited for our professor to show up. At a lull in the conversation, I wondered out loud what might be the most common disease, the "Number One Killer"? It seemed that we should be giving that one - whatever it was - more attention than the zebras that seemed to be on everyone's mind. (Okay, maybe I was swimming upstream here, but it wouldn't have been the first time - nor would it be the last.) Surprisingly, no one knew. Our intern showed up, so we asked her, but she didn't know either. I went home and pored over my fat medical textbooks (there was no Google box back then) until I found the answer: atherosclerosis. Hmmm. We had been seeing a lot of heart attacks, strokes, and peripheral vascular disease.
Now, forty-plus years later - with an impressive array of medical discoveries behind us and even more ahead - guess what's still the most common disease?
Back then the plaques and heart attacks and strokes caused by atherosclerosis seemed to appear magically out of nowhere. We hadn't a clue about the etiology (the underlying causative mechanisms) of atherosclerosis. Now we do. Over the years since I was a medical student, researchers in cell biology and molecular medicine have painstakingly unraveled this incredibly complex puzzle. Thousands of pieces have fallen into place, and medical science has finally achieved a thorough understanding of the complex sequence of events that culminates in a heart attack or a stroke. We now understand why arteries harden, how plaque forms, and what causes the blood clots that block arteries and kill or disable people by the millions. Researchers have identified the key biochemicals that cause atherosclerosis and it is now possible - even easy - to test for these markers to determine your atherosclerosis risk.
As our molecular biological understanding of atherosclerosis has matured, parallel research in nutritional biochemistry has revealed a diverse array of natural agents that block and reverse the causes of atherosclerosis. All are molecules normally present in the body, and, as such, they are experienced as "friendly". These food-derived medicines-herbs, enzymes, hormones, vitamins, minerals, essential fatty acids, amino acids, food extracts, and phytopharmaceuticals (plant-derived medicines) - "belong" in your body and your body instantaneously knows it. Those "friendly" natural medicinal substances are managed by your biochemical systems as if they were - and indeed, in most cases they actually are - real food. We call this "biocompatibility". Drug medicines are not biocompatible and predictably elicit toxic reactions. Pharmaceutical medicines trigger cellular reactions designed to "detoxify" - in other words, "kick out the culprit". This is why drugs almost invariably have side effects, toxic reactions, and other signs of incompatibility. Natural nutritional medicines don't do that.
Beyond biocompatibility, there's another huge reason natural medicines are preferable to drugs. While pharmaceuticals exert their effects by suppressing symptoms, natural medicines actually support and nourish the healing process.
Let me give you a few quick examples of natural medicines that prevent and reverse heart disease. Pomegranate juice reverses atherosclerosis. Methylfolate (a B-complex vitamin) prevents the homocysteine accumulation that irritates and damages blood vessels. Red yeast rice extract, a Chinese Traditional herbal medicine, lowers cholesterol and C-reactive protein gently and naturally. Curcumin, the active ingredient in the spice turmeric, reverses inflammation and discourages excess blood clotting. Nattokinase, an enzyme derived from soy, gently dissolves the clots that block blood vessels. Green tea extract, a powerful antioxidant, lowers cholesterol and prevents endothelial damage. Serrapeptase, another enzyme, dissolves atherosclerotic plaque and blood clots. I could go on and on - and I will, later in this book.
Unfortunately, there's a huge disconnect between these research findings and their clinical application. Doctors simply don't know about this stuff. Even though simple nutritional medicines like pomegranate juice, green tea, and turmeric have been shown beyond any doubt to address and reverse the molecular biological causes of atherosclerosis, physicians continue to prescribe a complex array of symptom-suppressing drugs and surgical techniques - Band-Aids that don't cure anything.
Why is the average doctor oblivious to these powerful healing agents? One must wonder whether the profit motive plays a role. After all, food-based medicines are unpatentable and therefore unprofitable. The dark political and economic forces that drive our dysfunctional health care delivery system work hard to suppress the free flow of information about natural medicines. But, really, those forces are beyond the scope of this book. Suffice it to say that we need a system where drug and insurance companies are not running the show. I believe most of us would welcome a shift away from the profit motive and back toward patient care - the kind exemplified for me when I was 16 by Dr. Hess.
Don't hold your breath. There are few signs of imminent change. While we wait, we need to be proactive, which - in terms of The "Number One Killer" - means get tested, and, if your markers are abnormal, follow the recommendations in this book. Atherosclerosis can be prevented, and even advanced disease can be reversed. It is exceedingly unlikely that your doctor knows this yet. Can you - can any of us - afford to wait until he or she figures it out?
I often think about my poker buddy Dwight, who, in 1981, was diagnosed with severe stenotic arteriosclerotic coronary artery disease. Dwight's left anterior descending artery had become completely obstructed by plaque. Bypass surgery - nicknamed CABG for Coronary Artery Bypass Graft (pronounced "cabbage") - was his only option. Dwight's surgeon, Dr. Stanley Morgan, invited me to scrub in.
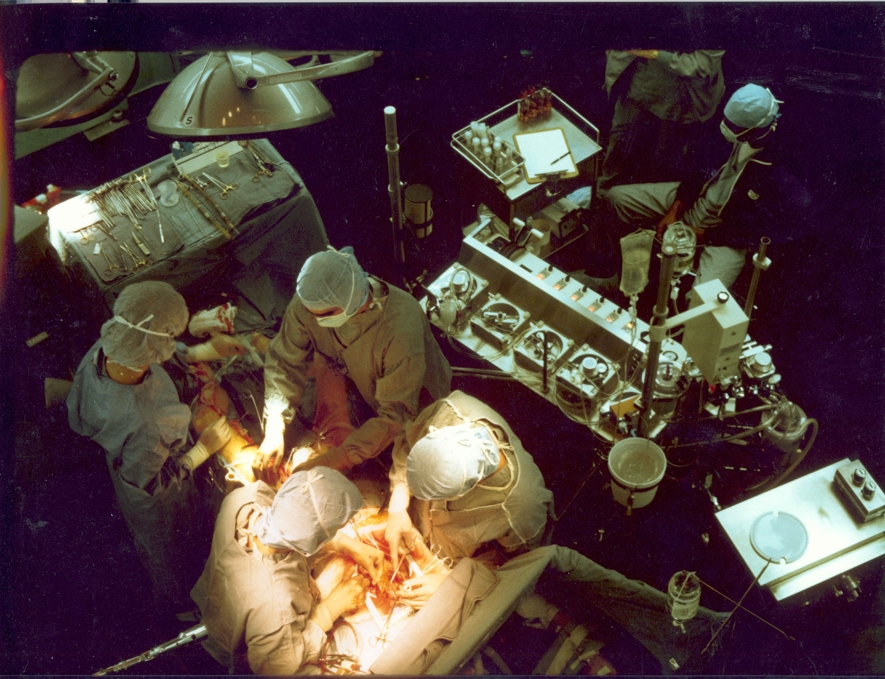
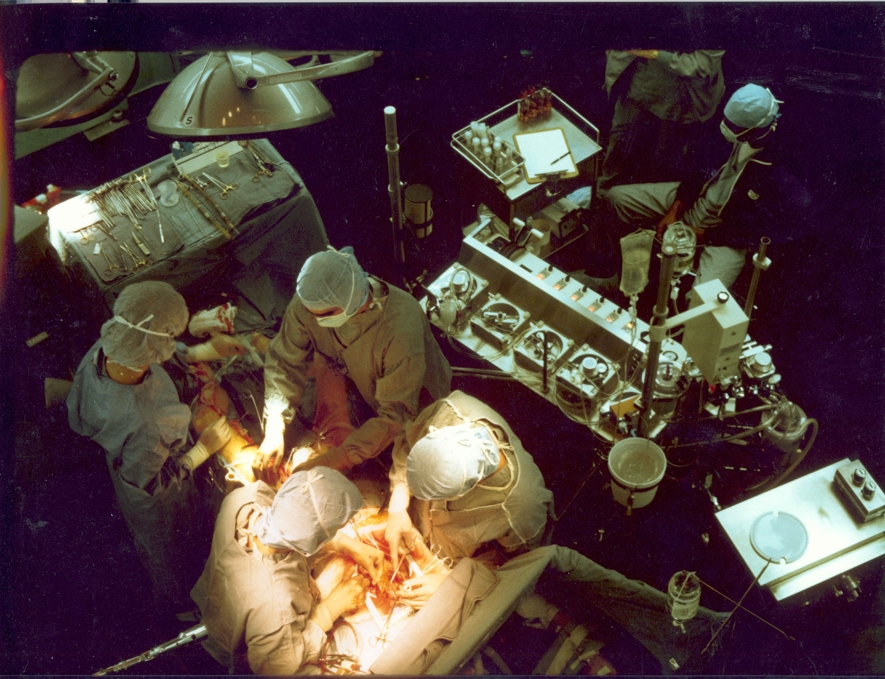
Two days later I found myself gowned, gloved, and backing through the OR door, hands held high. In the center of the room on the surgical table lay Dwight, bare-chested under bright lights, prepped and thoroughly anesthetized. He was fully anesthetized and unconscious. At his side stood Dr. Morgan, going down his pre-op checklist. He glanced up and gave me a quick, "Hi, Tim," then went back to his preparations.
I was greeted cheerfully by Dr. Ben Jones, the perfusionist, whose job was to keep Dwight's blood circulating while the surgeon worked on his heart.
"What kind of music do you like?" he asked.
"That's an odd question," I thought. Sensing my confusion, he pointed at the controls of a high tech stereo system built-into his command console. The cardiopulmonary bypass machine featured a state-of-the-art sound system complete with compact cassette.
"These procedures can take four, six, even eight hours, and good music helps us pass the time."
"Oh. Well, I like both kinds," I quipped, "country and western". He gave me a funny look, so I quickly added, " ... but I'm eclectic. Anything's okay." (Hip-hop and rap hadn't yet been invented or I might have had to make some exceptions.) "How about classical?"
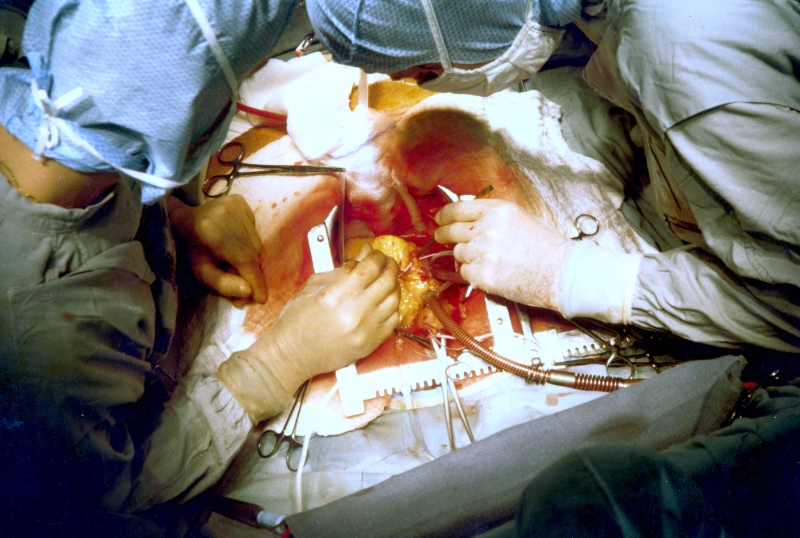
Dr. Morgan made sure everyone was ready, then put his scalpel to Dwight's chest and swiftly made a long, deep vertical midline incision that exposed the breast bone. "Sternal saw, please."
The acrid, nauseatingly familiar odor of instantaneously vaporized flesh washed over us as Morgan sliced deeper and deeper into Dwight's chest. In a few minutes Dwight's pericardial sac was exposed to the bright surgical lights. Dr. Morgan gently slit it open with his scalpel, exposing Dwight's beating heart.
It's hard to do surgery on a moving object. To stop the heart from beating, Dr. Morgan injected 500 cc of potassium chloride into the aortic root. Two more beats and Dwight's heart stopped cold. I looked up at the EKG monitor and noticed the flat line.
Dr. Morgan now quickly hooked up the heart-lung machine that would cool, oxygenate and pump Dwight's blood until the obstructed coronary artery could be removed and the bypass graft stitched into place.
It's more than a little creepy to gaze into a friend's open chest and view his exposed heart. That had stopped beating. Technically, my friend Dwight was dead.
As Dr. Morgan accessed Dwight's heart, a second surgeon, Dr. Hale, had been carefully dissecting (we call it "harvesting") his saphenous (leg) vein, the piece of living tubing that would replace the blocked anterior descending coronary artery. Dr. Hale now gingerly handed the piece of vein to Dr. Morgan who then meticulously stitched it into place.
Dwight's heart was then restarted. The big concern at this stage was a leak in the stitching when blood pressure returns to the heart, and we breathed a collective sigh of relief when Dwight's sutures all held.
Dr. Morgan wired Dwight's sternum back together and sutured the skin back in place over it. Four hours of intense concentration, but now he was done. He pulled off his gloves and took a deep slow breath.
Bypass surgery has come a long way since Dwight's procedure. The new cardiology sports a high-tech and amazing array of options including endoscopy, angioplasty, valve replacements, stents, and creative new imaging techniques. I have nothing but awe and respect for the incredible skills and dedication of cardiologists, cardiovascular surgeons, anesthesiologists, and perfusionists - a hardworking and committed breed of doctor. They save thousands of lives. Yet nothing would make me happier than to put them out of business. Research shows this can be done. It's time to apply what we know and make the leap from high-tech barn door closing to prevention and reversal. This book will explain how.
As the astonishing life and death drama of Dwight's bypass operation unfolded before my eyes, I couldn't help but wonder how things had gotten so bad for him (and millions like him) that all this technology and surgical skill had become necessary. I remember thinking there must be a way to head this off at the pass. But what was it? Another quarter century would pass before researchers would fully unearth the molecular biological causes of atherosclerotic coronary artery disease, but now we do have a definitive picture. The disease is now curable. Parallel developments in nutritional biochemistry have provided dietary information and an armamentarium of natural nontoxic medicines that address - and reverse - the causes of the disease.
Late afternoon the next day I returned to the hospital and rode the elevator up to the Intensive Care Unit to see Dwight. He was still a little groggy from the anesthesia, so I just stood there next to his bed, gazing at the monitors and thinking about yesterday. After a while he realized I was there.
"Hi Dwight. How are you doing?" I asked.
"Still in a fog, Tim - but, strangely, I've got more energy. I feel better."
This didn't surprise me. Due to the clogged vessels, Dwight's heart muscle cells had been suffering prolonged starvation. Now, thankfully, they were getting the nutrients and oxygen they needed.
"It must have been strange to be actually looking at my heart. That doesn't happen very often."
"Yeah," I answered, "as experiences go, I just can't pigeonhole that one."
"I guess they got it fixed up and running again, or we wouldn't be here chatting."
A lump swelled up in my throat. A short "Yup" was all I could manage.
Suddenly a stocky, white-gowned woman with a blank expression entered carrying a tray of food which she unceremoniously plunked down onto Dwight's bedside table. She skedaddled without a glance, a smile, or a word.
Dwight's first post-surgical meal! A little cloud of steam lifted off as he raised the cover. We both glanced at it, then at each other. First we frowned, then broke out in laughter. Oh my god! The irony was so thick you could cut it with a scalpel (or perhaps a butter knife). On the tray - and I am not making this up - sat a small, well-marbled overcooked steak with plenty of extra fat around the edge, perhaps harvested from a plaque-laden candidate for a bovine bypass in some parallel universe. Alongside the meat, four or five anemic canned string beans peered up at us. The "salad" consisted of a single leaf of lettuce on which sat a chunk of artificially colored (it had that "day-glo" look) green Jello, internally sprinkled with a few small pieces of canned pear. Beside the plate was a single slice of white bread and a pat of butter. Dessert was a little square piece of white cake topped with a buttery sugary frosting. The (by then well-established) connection between diet and heart disease had somehow eluded the nutritionist who assembled this culinary debacle that shouted up at us, "Want another heart attack? Just eat me."
As our scientific understanding of atherosclerosis has flowered, so, too, has our appreciation of the potent effects of various foodstuffs on arterial health. Even back in the early eighties when Dwight's surgery was done, we knew that certain foods (e.g., animal fat, white flour, refined foods, sugars, processed food, chemical additives, sugar, and saturated fat) encouraged atherosclerosis. As you'll see later in this book, subsequent research has revealed that many foods discourage and even reverse atherosclerosis. If an enlightened nutritionist had fashioned Dwight's post-surgical meal applying what we know today, it might have contained nuts, beans, and small portions of very lean meat - perhaps a stir fry or curry spiced with turmeric (which contains curcumin). Broccoli or artichoke or just about any vegetable. A salad with garlic, onion, leafy greens, tomato, carrot, and a dressing made with flaxseed oil and vinegar. Dessert might be fresh fruit. A glass of pomegranate juice or a cup of green green tea. There's an almost infinite number of possibilities of heart-protective foods to choose from - and you'll see lists of them in later chapters.
"Hey, Tim, wanna catch a Raider's game with me this weekend? It's free."
My buddy Donny - a fellow physician - was on the line.
"They need docs in the stands in case a fan needs medical attention. I've done it a couple of times already, Tim, and nobody's gotten sick so far. We'll probably just watch the game and then go home."
Seemed like a good deal to me, so - oblivious to how complicated my life was about to become - I said, "Sure."
Fast forward to a sunny Sunday afternoon at the Oakland Coliseum. It was 1978 and the Oakland Raiders were about to take on the Seattle Seahawks. After the head doctor briefed us, we lugged our emergency supply bag up to our free 50-yard line seats and relaxed - ready to go to work if necessary, but not expecting any excitement beyond what the game would generate. Early in the second quarter an usher shouted to us from the aisle. "Hey! Doc! Someone's real sick - right over there!" He pointed about twenty rows over, where we easily spotted the gentleman I will call "Mr. Raiders Fan" (we never did learn his real name), sprawled on the cement walkway beside his seat.
We grabbed our medical gear and dashed over. We got to him in just a few seconds but he was already unconscious and unresponsive. No pulse. No respiration. No diagnostic challenge here: Mr. Raiders Fan was having a heart attack. We immediately initiated CPR. Donny did the chest/heart compression while I tried in vain to insert the plastic airway. Mr. Fan's vomiting reflex frustrated my attempts to get a breathing tube in. As luck would have it, right at that moment a guy emerged from the crowd and huddled down next to us over the patient with some very welcome news.
"I'm an anesthesiologist and I can get that airway in for you."
"Great," I replied and quickly handed it to him. I moved aside and watched him successfully insert it on the first try. What a relief! Now Mr. Fan was able to get plenty of air.
At that point we felt we had a good chance of saving him.
The next day's Oakland Tribune featured a photo. The bottom half showed me, Donny, and the mystery anesthesiologist - backs to the camera - squatting over Mr. Fan's lifeless body. Above and behind us, facing the camera, were platoons of fans, standing up so they could see over us. Not a single person was looking down at us! None of them showed the slightest interest in the struggle to save a fellow human's life. I wonder if they'd have paid closer attention if they'd known their own odds of having a heart attack were roughly one in two - and the odds they' survive that attack were about the same.
After we had worked on Mr. Fan for a few more minutes, two paramedics arrived. Together we hefted Mr. Fan up onto a gurney and rolled him through the crowd and out to their ambulance, then sped off - sirens blaring - to Oakland's Highland Hospital, where, despite the best ER code blue technology ... well, the outcome was not good. Let's just say this was Mr. Fan's last hot dog, last beer, and last football game - and he would have been disappointed that the Raiders lost the game to the Seahawks - by a single point.
Mr. Fan had been dancing with death for quite a while. At the time, we couldn't explain why Mr. Fan had a heart attack, but now, 30 years later, with the wisdom of hindsight, it is safe to say that atherosclerotic vascular disease had been eroding his arteries - from the inside out - for decades. Assuming his case was typical, fatty yellow patches of atherosclerotic plaque covered much of his abdominal aorta by the time he was ten years of age. Now in his late forties, plaque had invaded the walls of many of his blood vessels, including those of his coronary arteries.
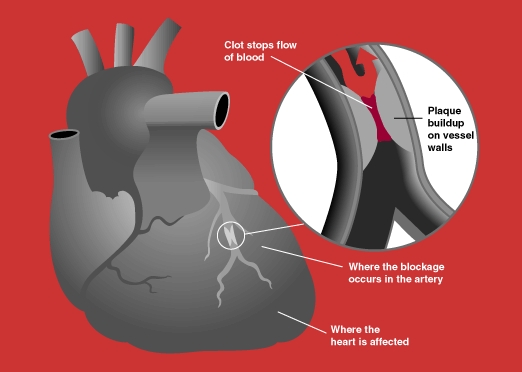
Most of the plaque deposited over the years in the walls Mr. Fan's vessels would have healed and hardened in place, and thus posed no immediate threat to his health. A small section of his anterior descending coronary artery (the main branch that supplies the left front of the heart), however, contained "unstable plaque," a fragile, incompletely healed scab-like affair that can easily break, causing local bleeding and clot formation. During the second quarter of the Seahawks game this unstable plaque burst like a broken pipeline, spewing out its contents. A large clot (or thrombus) quickly formed at the site of the rupture. This clot stopped the hemorrhage, but in the process created a bigger problem; it became a roadblock that prevented passage of crucial nutrients and oxygen to the heart muscle downstream. Within seconds, Mr. Fan's heart stopped beating.
Mr. Fan's condition was far from unique. Just about everybody in the western world has some degree of atherosclerosis. According to William P. Castelli, M.D., director of the renowned Framingham Heart Study, "About three quarters of the population of the USA older than 30 years has some lesion related to atherosclerosis in the arterial tree. This lesion gets worse almost every day in all these people and will eventually result in closure of a vital artery in half of them, causing their death." Mr. Fan was on the short list.
In 1978 we didn't know what caused atherosclerosis, and we didn't know why some atherosclerotic vessels broke and bled, while others didn't. Donny and I did know, however, that a blood clot had developed inside a major vessel in Mr. Fan's heart and was blocking blood flow through it. It would take researchers another quarter century to figure out exactly what triggers the formation of these cataclysmic clots.
Endothelial damage and dysfunction causes atherosclerotic plaque, heart attacks, and strokes
Now, with the wisdom of hindsight, it is safe to say that Mr. Fan's problems began and ended in his endothelium, the single layer of cells that lines the inside of all blood vessels. Discovered in 1973, the endothelium was originally thought to be passive and inert, and that oxygen, carbon dioxide and nutrients passively diffused through it. Nothing could be further from the truth. We have learned that the endothelium is a strategically-positioned, proactive organ that makes vital metabolic decisions and exerts powerful control over the farthest reaches of our bodies. The total length of your circulatory system is about 100,000 miles, every single one of which is lined with a continuous sheet of endothelial cells. Placed side-by-side, the endothelial cells from a single human would wrap more than four times around the circumference of the Earth. The total endothelial surface area is 4000-7000 square meters, which, if spread out flat, would cover roughly the same area as a football field.
The endothelium is a highly selective semi-permeable membrane that maintains internal order by deciding what stays in the bloodstream and what gets past it into the wall of the blood vessel (and then beyond to every organ and tissue in the body). The endothelium monitors and manages the transit of thousands of blood-borne entities - from the smallest molecules to large proteins to (relatively) huge white blood cells - into and out of the bloodstream. Though immune health and inflammation management - two key features of cardiovascular health - head up the list of functions that depend on endothelial health, one would be hard-pressed to find a bodily function not directly influenced by it. When damaged, the endothelium fails - and when it fails, bad things happen. Like Mr. Fan's heart attack.
Prolonged endothelial exposure to irritants causes atherosclerotic plaque, a kind of scar tissue that forms in the walls of vessels that are trying to heal from ongoing injury. Protecting your endothelium from damage is the first and most important step in outsmarting the "Number One Killer". The heart marker blood tests discussed in this book will detect the presence of endothelial damage - and even tell you what's causing it. This information, available for less than $200, is empowering because it tells you what is going to cause your heart attack or stroke. Then, by applying the information provided in this book, you can reverse it.
You'd think that an organ as large and important as the endothelium would be taken seriously by mainstream medical clinicians, but it's not. Endothelial damage, dysfunction, and failure causes the myocardial infarctions and strokes that account for the vast majority of mortality in the western world, but you'd have a hard time finding a doctor who could tell you what the endothelium is, much less what it does or why it's important. Finding a doctor - even a cardiologist - who could tell you how to fix a broken endothelium would be even more difficult. That kind of information is an important piece of "what your doctor is for" - so I will tell you, in this book, how to determine whether your endothelium is damaged, what damaged it, why that translates directly into cardiovascular disease risk, and how to make it healthy again.
Nutrition - what you do eat and what you don't eat - plays a powerful role in causing, preventing, and even reversing atherosclerotic vascular disease. A lifestyle laced with stuff on the above list will generate plaque. Avoiding these items will protect you against endothelial damage and atherosclerosis.
Most Americans have already developed advanced atherosclerotic heart disease. How can you determine whether you are among them? The disease is "silent," so you won't have symptoms or signs (like chest pain or shortness of breath) to alert you. This is where state-of-the-art biochemical medicine comes in handy. Lab testing - specifically a fasting blood sugar, C-reactive protein, homocysteine, fibrinogen, and a lipid panel - will tell you whether endothelial dysfunction and plaque are busily at work eroding your arterial health. And if they are, diet and natural medicines can and will reverse it. I'll provide a lot more detail about this in later chapters, but I want to start by telling you how I would have treated Mr. Fan if he had come into my office a month or two before the Seahawks game (assuming we knew then what we know now).
After a thorough history and physical examination, I would have ordered the above-listed tests. Then, while waiting for the test results, I would have prescribed four remarkable nutritional medicines, each of which will reverse atherosclerosis regardless of cause: pomegranate juice, curcumin, nattokinase, and serrapeptase.
(Most doctors, when confronted with coronary artery disease, are so heavily programmed to prescribe drugs like statins, beta blockers, and anticoagulants that they are unaware of the huge array of powerful nontoxic nutritional medicines that accomplish something no drug can do: reverse atherosclerosis. This is not a casual statement; it is supported by thousands of peer-reviewed scientific studies published in the scientific literature. See References.)
Mr. Fan's pomegranate juice must be pure, unadulterated, and organic. This delicious sweet ruby red juice melts away atherosclerotic plaque and encourages damaged endothelial membranes to heal. It lowers cholesterol by blocking synthesis in the liver, lowers blood pressure (risk factor for heart attacks), and exerts a gentle natural anticoagulant effect that reduces the risk of vessel-blocking blood clots (kind of like baby aspirin but without being an irritating foreign chemical). If that weren't enough, pomegranate juice is the most powerful fruit-derived antioxidant, and has been shown to reduce oxidative stress everywhere in the body. This incredibly versatile food also blocks osteoporosis, beefs up immune function, and provides potent protection against breast, prostate, and colon cancer. And it tastes great!
The anti-inflammatory herb curcumin (the active ingredient in the curry spice, turmeric) blocks initiation and progression of atherosclerotic plaque. Best provided in combination products containing supportive anti-inflammatory herbs such as rosemary, holy basil, green tea, ginger, coptis, barberry, skullcap and Protykin, curcumin lowers cholesterol, LDL, fibrinogen, and C-reactive protein; it reverses endothelial damage, protects LDL from being oxidized, and prevents blood clots like the one that killed Mr. Fan. Because curcumin is poorly absorbed, stick with turmeric "phytosome" products in which the curcumin has been bonded to a carrier molecule, usually phosphatidylcholine.
The third nutritional heart medicine I'd recommend is serrapeptase (Serralase), an anti-inflammatory enzyme that reverses atherosclerosis by dissolving away the fibrin scaffold upon which plaque is deposited. Serrapeptase also digests and removes thrombi, those artery-blocking blood clots (again, constructed from the fibrin generated by fibrinogen). Originally discovered centuries ago by Chinese Traditional Medicine herbalists, serrapeptase is the enzyme secreted by the silkworm moth to digest its way out of its cocoon. The modern version is cultured from bacteria, purified, and made into a tablet.
After I got Mr. Fan started on a program of nutritional medicines to reverse his heart disease, we'd have some long chats about dietary choices. I'd recommend fresh whole foods and a low carb (minimal grains and no sugars) diet. Though small portions of lean meat are acceptable, the main focus needs to be on vegetables, fruit, beans, nuts, and seeds.
In the short run, yes, it might be easier to use drugs to suppress Mr. Fan's symptoms, but I'd rather put the principals of molecular biology to work removing the causes of his heart disease. Our understanding of the fundamental science behind atherosclerotic plaque - coupled with an appreciation of the biochemistry of nutrition - now make that possible. Mr. Fan was born a quarter century too soon.