Print Files: A4 Size (pdf), Text (txt).
The purpose of this work consisted of quantitative studies of the effects caused by ionizing radiation on the materials commonly used in dental restorations (amalgam, composite resin and compomer), to mitigate the deleterious effects of radiotherapy when patients with tumors in head and neck, observed when the teeth are restored within the field of radiation. Samples were submitted to the beam of radiation from a source of cobaltoterapia, and analyzed by a X-ray fluorescence technique, by comparing the chemical composition of samples before and after irradiation. Gamma spectrometry was performed with detector of NaI and HPGe in the same samples. Then, the samples were kept in an appropriate place and after 8 years is repeated the same analysis.
With these tests, it was possible to verify small changes in the composition of bodies of evidence due to the interaction 8 years after exposure to gamma radiation beams, simulating a patient who develops deleterious effects of radiation after the end radiotherapy treatment.
This work is consisted in quantitative studies of the effects of ionized radiation under materials used in dental restorations (amalgam, resin-based composite, and compomer) aiming at brighten up the possible deleterious effects of the radiotherapy for patients with head and neck tumors if the dental restoration is inside the radiation field. Test bodies were submitted to a gamma-ray beam from a cobalt therapy source. They were analyzed using a X-ray fluorescence technique and their chemical composition, before and after the irradiation, were compared. Gamma ray spectrometry with Sodium Iodate (NaI) detectors was also done using the same samples. After this, the samples were conserved in a proper place and, 8 years later, the same analyses were repeated.
From these analyses, it was possible to verify small changes in the chemical compositions of the test bodies due to their interaction with radiation and, comparing the results obtained 8 years after the exposition to a gamma ray beam, it was also possible to simulate a patient that develop deleterious effects of radiation after ending the radiotherapy treatment.
Currently, there are several types of restoration materials. In this work, three of the most commonly used materials were studied: the amalgam, the resin-based composite, and the compomer [10],[11].
Deontological studies correlate the emergence of caries in patients that were submitted to radiotherapy [18],[15]. In general, caries due to radiation show different aspects, their evolution is fast and painless, and they appear around three months after ending the radiotherapy treatment. They affect all the dental surfaces and are related to the xerostomy and the changes in the food habits [16],[17]. Nowadays, techniques to prevent this type of caries include topical application of Fluor, mouths washing with fluorinated substances and use of fluorinated dental cream [9],[4].
Before beginning a radiotherapy treatment, the patient should be submitted to a dental evaluation and the dentist should elaborate a fast and efficient treatment that include the extraction of residual dental roots, the treatment of cariously injuries, the elimination of periodontal problems, and the correction of malocclusions (also teeth badly located that are causing trauma in the buccal cavity). This way, the buccal healthy is given back to the patient to aim do not aggravate his or her problems during the oncologic treatment. In the cases these previous treatments are not possible, the dental extraction is recommended [6],[14]. Once established caries due to radiation, the treatment consists in restoration using fluorinated materials, amputation of the dental crowns and confection of prosthesis [14],[19]. In these cases, the patients are submitted to alternative therapies, but only with the palliative purpose of relieving the symptoms [8].
For this reason, it is extremely important the development of researches that investigate the real effects of radiation under the human teeth and that look for alternatives to brighten up or eliminate the deleterious effects of radiotherapy in patients with mouth tumors.
The main goal of this work is to study the possible chemical composition alterations of the materials cited above after submitting them to a gamma-ray beam. For this purpose, X-ray fluorescence technique and gamma spectrometry were used and the results obtained in 2001, when the first analysis was carried out, were compared to the results obtained in 2009 for the same materials.
The analyzed samples were confectioned and divided in three sets: set 1 corresponds to the amalgam samples, set 2 to the resin-based composite samples, and set 3 to the compomer samples.
The test bodies were distributed in two groups: a pilot group which contains 5 samples from each one of the sets 1, 2, and 3 that were not submitted to radiation, and another group with 15 samples from each set that were irradiated.
The pilot group was analyzed by the X-ray fluorescence technique to discriminate the exact chemical composition of the materials to be irradiated, since each chemical element has its own response to radiation. Once their chemical composition were known, the samples of the group to be irradiated were submitted to a gamma-ray beam from a cobalt therapy source. The dose was from 5000 to 7000 GCi, which represents the dose received (i.e. the average dose from treatment protocols) by patients with head and neck tumors submitted to cervical or facial radiotherapy that covers a great part of the dental arcade. In fact, the treatment dose is 180 GCi per day, 5 days per week. The case analyzed here corresponds to the situation of greater intensity of the acute and chronic radiobiological effects.
Following this procedure, the irradiated samples were submitted to gamma spectrometry using a Sodium Iodate (NaI) detector in 2001 and a Hyper Pure Germanium (HPGe) detector in 2009. The goal of this analysis was to determine the photon counts of the energy peaks of the irradiated samples and to verify if there was any difference in their emission compared to the pilot sample (i.e., not irradiated sample).
The chemical composition of the irradiated samples was obtained by the X-ray fluorescence technique and the results were compared to those of the pilot sample.
After this, the samples were conserved in a proper place and 8 years later the same analyses were repeated and the results were compared.
Comparison between the results of 2001 and 2009 for the chemical composition determined by the X-ray fluorescence technique (before and after the irradiation).
| Present Element | Pilot samples analyzed in 2001 | Irradiated samples analyzed in 2001 | Pilot samples analyzed in 2009 | Irradiated samples analyzed in 2009 |
| Abundance % | % | % | % | % |
| Hg | 53,5 ± 0,01 | 53,9 ± 0,01 | 42,4 ± 0,7 | 45,5 ± 0,7 |
| Ag | 23,3 ± 0,01 | 23,3 ± 0,01 | 25,9 ± 0,7 | 23,9 ± 0,8 |
| Sn | 14,6 ± 0,01 | 14,1 ± 0,01 | 13,6 ± 0,9 | 18,8 ± 0,9 |
| Cu | 7,3 ± 0,01 | 7,6 ± 0,01 | 11,0 ± 0,1 | 9,9 ± 0,1 |
| Si | 0,49 ± 0,01 | 2,2 ± 0,2 | 1,9 ± 0,1 | |
| Zn | 0,17 ± 0,01 | 0,092 ± 0,01 | ||
| Al | 0,11 ± 0,01 | |||
| Cr | 0,094 ± 0,01 | 0,067 ± 0,01 | ||
| Fe | 0,084 ± 0,01 | 0,096 ± 0,01 | ||
| P | 0,045 ± 0,01 | |||
| Ni | 0,039 ± 0,01 | 0,020 ± 0,01 | ||
| Co | 0,022 ± 0,01 | 0,036 ± 0,01 | ||
| Na | 0,50 ± 0,01 | |||
| Mn | 0,022 ± 0,01 | 0,071 ± 0,01 |
| Present Element | Pilot samples analyzed in 2001 | Irradiated samples analyzed in 2001 | Pilot samples analyzed in 2009 | Irradiated samples analyzed in 2009 |
| Abundance % | % | % | % | % |
| Si | 40,1 ± 0,01 | 37,8 ± 0,01 | 26,7 ± 0,1 | 25,1 ± 0,1 |
| O | 33,1 ± 0,01 | 37,8 ± 0,01 | 37,2 ± 0,1 | 37,1 ± 0,1 |
| Zr | 24,2 ± 0,01 | 23,3 ± 0,01 | 30,4 ± 0,1 | 33,8 ± 0,1 |
| Hf | 0,73 ± 0,01 | 0,57 ± 0,01 | 0,57 ± 0,1 | |
| Al | 0,48 ± 0,01 | 0,35 ± 0,01 | ||
| Na | 0,45 ± 0,01 | 0,33 ± 0,01 | ||
| Cal | 0,35 ± 0,01 | |||
| Cl | 0,21 ± 0,01 | 0,27 ± 0,01 | ||
| Co | 0,006 ± 0,01 | |||
| S | 0,17 ± 0,01 | |||
| P | 0,072 ± 0,01 | 0,057 ± 0,01 | ||
| Mg | 0,064 ± 0,01 | |||
| Fe | 0,057 ± 0,01 | 0,050 ± 0,01 | 0,09 ± 0,01 | 0,062 ± 0,01 |
| Cu | 0,008 ± 0,01 | 0,004 ± 0,01 | ||
| Ni | 0,006 ± 0,01 | 0,009 ± 0,01 | ||
| Mn | 0,003 ± 0,01 | 0,012 ± 0,01 | ||
| Cr | 0,002 ± 0,01 | |||
| Zn | 0,001 ± 0,01 | |||
| Ca | 0,8 ± 0,1 |
| Present Element | Pilot samples analyzed in 2001 | Irradiated samples analyzed in 2001 | Pilot samples analyzed in 2009 | Irradiated samples analyzed in 2009 |
| Abundance % | % | % | % | % |
| Sr | 34,9 ± 0,01 | 43,2 ± 0,01 | 72,7 ± 0,01 | 0,16 ± 0,01 |
| O | 29,0 ± 0,01 | 24,9 ± 0,01 | 19,5 ± 0,01 | 45,7 ± 0,01 |
| Si | 15,7 ± 0,01 | 17,0 ± 0,01 | 33,9 ± 0,01 | |
| Al | 8,6 ± 0,01 | 9,7 ± 0,01 | 6,9 ± 0,01 | |
| F | 6,6 ± 0,01 | |||
| P | 2,1 ± 0,01 | 2,6 ± 0,01 | ||
| Na | 1,6 ± 0,01 | 1,6 ± 0,01 | ||
| Ca | 0,46 ± 0,01 | 0,46 ± 0,01 | ||
| Cl | 0,36 ± 0,01 | 0,28 ± 0,01 | ||
| S | 0,28 ± 0,01 | 0,14 ± 0,01 | ||
| K | 0,23 ± 0,01 | |||
| Fe | 0,085 ± 0,01 | 0,030 ± 0,01 | 0,042 ± 0,01 | |
| Mg | 0,078 ± 0,01 | |||
| Mn | 0,023 ± 0,01 | 0,025 ± 0,01 | ||
| Cu | 0,016 ± 0,01 | 0,015 ± 0,01 | ||
| Co | 0,013 ± 0,01 | 0,009 ± 0,01 | ||
| Ni | 0,010 ± 0,01 | 0,012 ± 0,01 | ||
| Cr | 0,017 ± 0,01 | |||
| Zr | 19,9 ± 0,01 | |||
| Hf | 0,4 ± 0,01 | |||
| Ba | 0,098 ± 0,05 |
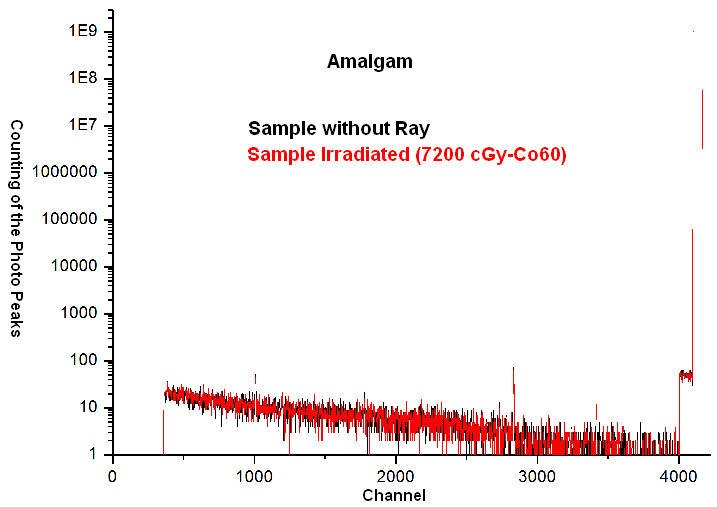
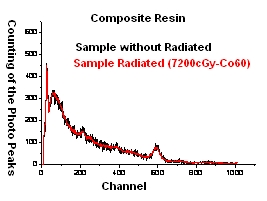
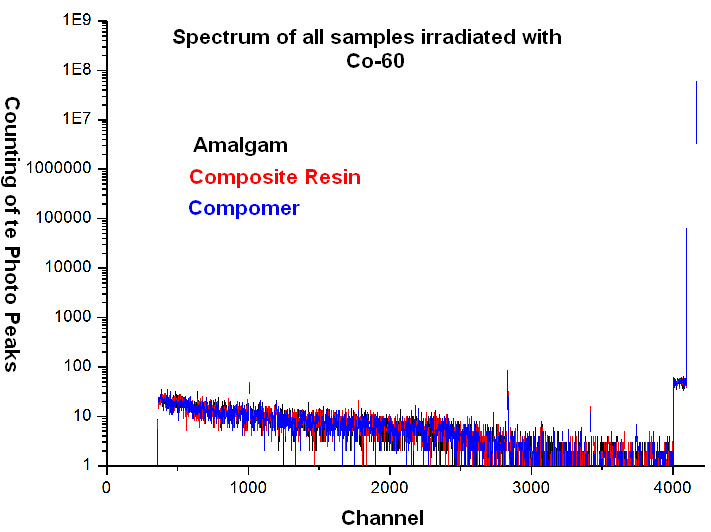
Photon counting of the energy peaks using the NaI detector in 2001 and the HPGe detector in 2009.
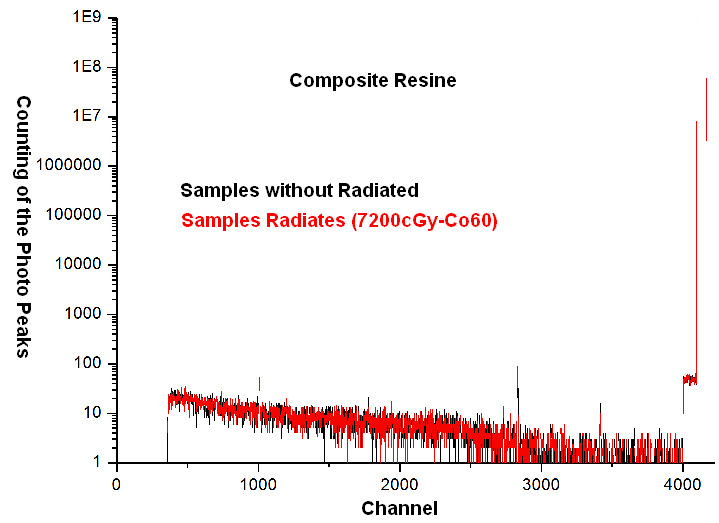
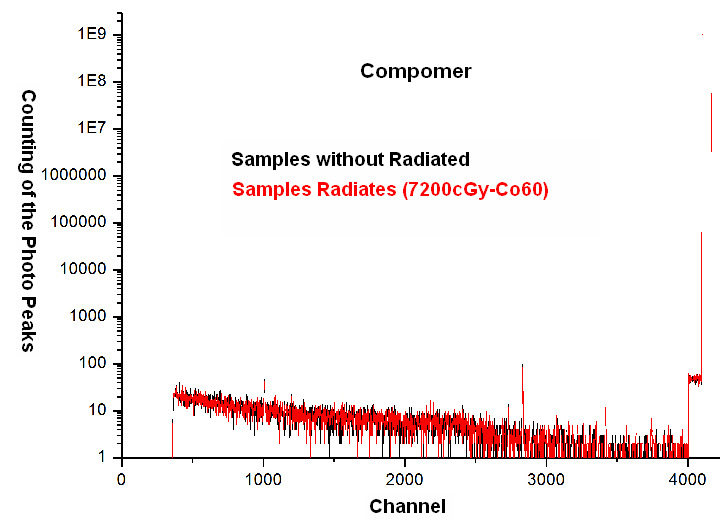
The irradiated and the non-irradiated samples were reanalyzed with equipments of gamma-ray spectrometry in order to verify changes in the photon counting of the energy peaks present in the sample as function of the radiation dose used. The gamma-ray spectrum was obtained for all test bodies using multichannel detectors (NaI in 2001 and HPGe in 2009). The behavior of the photon-peaks as function of the energy of the radiation (i.e., the instrument channel) is shown in Figures 1, 2 and 3 for the amalgam, resin-based composite, and compomer samples respectively. These Figures contain the two analyses of the material, the first one of 2001 and the second one of 2009. The counting time in both cases was 1800 seconds.
The following Figures illustrate the gamma-ray spectrums (NaI and HPGe detectors) of the three types of irradiated samples.
In tables 1 and 2 it is noted that there was no significant changes. The elements that disappear in 2009 are of low abundance in 2001 and can not be characterized in the laboratory for analysis in 2009.
In table 3, there are significant changes in the samples. But further analysis is needed for more accurate conclusions.
In figures 1, 2 and 3, you may notice that showed no residual radiation when irradiated in 2001 and reviewed in 2009.